Key findings from a study on families experiencing homelessness
Family lens: Family Wellbeing
Research Snapshot: Housing Shortage as a Driver for Family and Household Change
Key findings from a study on how rising housing costs and limited housing supply shaped families and households in large Canadian cities
“Who Is Family and Why Should We Care?”: A Conversation About Family Diversity and Wellbeing
As part of our 60th anniversary, the Vanier Institute of the Family recently partnered with the Department of Human Ecology at the University of Alberta to host the panel discussion “Who Is Family and Why Should We Care?”
Research Snapshot: The Complex Impact of Medical Assistance in Dying on Families
Research Snapshot: Exploring Lived Experiences of Pain in Military Families
Research Snapshot: Indigenous Care Leavers Aging Out of Care in Manitoba
Highlights from a study about how Indigenous children are overrepresented in the child welfare system in Canada
Research Snapshot: Queer Households and Possibilities for Shared Housing in Canada
Highlights from a study about housing policies and 2SLGBTQI+ families
Research Snapshot: Children in Out-of-Home Care in Canada: Insights from Administrative Data
Highlights from a study about the number of children in out-of-home care in Canada
Research Snapshot: Newcomer Women’s Experiences of Intimate Partner Violence in Canada
Highlights from a study about newcomer women’s experiences of family violence
Research Snapshot: Families with Refugee Backgrounds Rebuilding New Lives in Saskatchewan
Highlights of a study on what contributed to refugees’ resilience after resettling in Regina, Saskatchewan
Issue Brief: Considering Families in Canada’s Digital Transformation
An overview of how technological change relates to inequalities within and between families
Research Snapshot: The State of LGBTQIA2S+ Military Family Research in Canada
Research Snapshot: The Relationship Between Fathers’ Social Media Use and Their Food Parenting Practices
Highlights of a study of how parents use social media and how it relates to their parenting practices around food
Issue Brief: Families, Disability, and Wellbeing in Canada
An overview of the wellbeing of families with disabilities in Canada
Research Snapshot: Peer and Family Belongingness Impact on the Mental Health of Black LGBTQ+ Youth
Highlights from a study about family support and Black LGBTQ+ youth
Research Snapshot: Inuit Mothers’ Visions for Child and Family Wellness in Nunavut, Canada
Summary of a study on how the child welfare system is perceived by Inuit mothers
Research Snapshot: Policy Change Impacts on Food Insecurity in Northern Canada
Summary of a study on the impact of the transition from the Food Mail Program to Nutrition North Canada on both Indigenous and non-Indigenous families
Research Snapshot: Motivations and Challenges for Grandparent–Grandchild Outdoor Play in Early Childhood
Summary of a study on the perspectives of grandparents regarding outdoor play with their young grandchildren.
UN Report: Interlinkages Between Demographic Change, Migration, and Urbanization in Canada: Policy Implications
An overview of policy implications on demographic change, migration, and urbanization in Canada
Research Snapshot: Homelessness Among Newcomer Families in Canada
Summary of a study on homelessness among immigrant families
Research Snapshot: Maternal Labour Force Participation and Separation Anxiety Among Children
Findings from a study about working mothers and separation anxiety among children
Research Snapshot: Protecting Against Food Insecurity: Impacts on Mental Health and Wellbeing
Summary of a study on protecting children from food insecurity
Research Snapshot: Spousal Bereavement and Adjustment Among Older Chinese Immigrants
A summary of a study on bereavement among immigrant families
Research Snapshot: Parents, Homeschooling, and Relationship Conflict During COVID-19
Highlights from a study on how providing homeschooling during COVID affected parents
Research Snapshot: Immigrant Men, Racism, and Family Wellbeing in Canada
Highlights from a study exploring the impact of the migration process in Canada on family wellbeing
Research Snapshot: Housing Affordability and Homeownership Among Immigrant Families in Canada
Key findings from a study on immigrant families and housing
Infographic: Employed Caregivers at Higher Risk of Negative Outcomes
Research on Aging, Policies and Practice has published new data on how caregiving affects employed Canadians.
Research Snapshot: Examining Benefits and Barriers to Participating in Family Physical Activity
Highlights from a study about families and active leisure
Migration and Urbanization Trends and Family Wellbeing in Canada: A Focus on Disability and Indigenous Issues
A report prepared for Expert Group Meeting on megatrends and families
Spouse or Significant Other Wellbeing Course: Supporting Public Safety Personnel Families
A profile of a wellbeing course for the spouses or significant others of PSP.
Research Snapshot: Parent–Child Separations Among First Nations and Métis Families
A summary of a recent study on the impact of parent–child separations on First Nations families
National Grandparents’ Day: New Insights from Canadian Research
A roundup of new insights and research on grandparents in Canada.
Research Snapshot: Gender, Affordable Housing, and the “Poverty Gap” in Canada
Highlights from a study on the experiences of women in Calgary who live in affordable housing
Research Snapshot: Access to Postnatal Healthcare and Supports Among Syrian Refugee Mothers
Findings from a study on the postnatal experiences of Syrian refugee mothers in Canada.
Research Snapshot: Impact of Maternal Incarceration on Family Relationships
Findings from a recent study of the effects of incarceration on mothers and their children.
Research Recap: Wellbeing of Middle-Aged and Older Adults Without Partners or Children
Dr. Rachel Margolis shares new research on the well-being of older adults without close kin.
Researcher Spotlight: Kim de Laat
Kim de Laat discusses her research on family diversities, inequality and parental leave.
COVID-19 IMPACTS: Newcomer and Refugee Mothers in Canada – Final Report
Final report on COVID-19 IMPACTS: Newcomer and Refugee Mothers in Canada survey.
In Conversation: Emily Glossop-Nicholson on Home as Family, Community and Connection
Emily Glossop-Nicholson discusses themes from her book Our Family Is Grateful.
COVID-19 IMPACTS: Family Therapists Survey – Final Report
Final report on the findings from the COVID-19 IMPACTS: Family Therapists Survey.
Timeline: 50 Years of Families in Canada (1971‑2021)
Learn about how families and family experiences in Canada have changed over the past 50 years with our new timeline!
Stories Behind the Stats: Becoming a New Dad During Lockdown
A conversation with a new dad about his journey into fatherhood during lockdown.
In Brief: COVID-19 IMPACTS Through a Gender-based Lens
Diana Gerasimov summarizes new findings on the gendered impacts of the pandemic.
Caregiving During COVID: What Have We Learned? (Video)
Alex Foster-Petrocco shares takeaways and highlights from a recent webinar on caregiving and technology during COVID-19.
REVIEW: Mothers, Mothering, and COVID-19: Dispatches from a Pandemic
Alex Foster-Petrocco reviews a new book exploring the experiences of mothers during COVID-19.
Report: Family Well-being in Canada
New report on well-being in Canada co-authored by staff from Statistics Canada and the Vanier Institute.
In Brief: Stressful Life Events and Food Insecurity
Diana Gerasimov shares data on the association between stressful life events and food insecurity.
In Brief: COVID-19 IMPACTS on Families Living with Disabilities
Vanier Institute’s In Brief Series: Mobilizing Research on Families in Canada
Diana Gerasimov
March 9, 2021
STUDIES:
Yang, F., K. Dorrance and N. Aitken. “The Changes in Health and Well-being of Canadians with Long-term Conditions or Disabilities Since the Start of the COVID-19 Pandemic,” StatCan COVID-19: Data to Insights for a Better Canada, Statistics Canada Catalogue no. 45-28-0001 (October 7, 2020). Link: http://bit.ly/3bXpkSh.
Arim, R., L. Findlay and D. Kohen. “The Impact of the COVID-19 Pandemic on Canadian Families of Children with Disabilities,” StatCan COVID-19: Data to Insights for a Better Canada, Statistics Canada Catalogue no. 45-28-0001 (August 27, 2020). Link: http://bit.ly/2QSNVxH.
Over the past year, the COVID-19 pandemic has negatively affected many Canadians’ physical and mental health,1 including limiting their access to services they may have otherwise reached out to for support. This can have a significant impact on those living with disabilities or long-term conditions, who are more likely to use health services on a regular basis and whose situation may be compounded by isolation and distance from familiar, informal social support.
In a recently published data from Statistics Canada, Canadians living with disabilities or long-term conditions who participated in a crowdsourced survey, from June to July 2020, reported declining health and mental health, as well as disruptions to health services. Variations in the general health of participants depend on the type of disability or long-term condition that individuals experience.
- 48% of participants living with disabilities or chronic conditions reported that their health was “somewhat worse” or “much worse” since before the pandemic.
- 64% of participants with cognitive conditions reported that their health had gotten “much” or “somewhat” worse compared with before the pandemic.
- 60% of individuals with mental health conditions reported that their overall health had gotten “much” or “somewhat” worse compared with before the pandemic.
- 48% of participants with hearing conditions reported their health to have stayed about the same.
- 73% of participants with mental-health related conditions reported “much worse” or “somewhat worse” mental health.
- 57% of participants with disabilities or chronic conditions self-rated their overall mental health as having declined since the beginning of the pandemic, while 36% reported that their mental health had not changed and 7% reported an improvement in their mental health (“somewhat better” or “much better”).
- 44% participants with hearing conditions reported consistent mental health since before the pandemic.
Families of children with disabilities
Another crowdsourced survey, which explored the experiences of parents of children living with disabilities, found that they were more likely to express concern for their children regarding their child’s mental health, anxiety and emotions, academic success and the impact of social isolation.
- 60% of parents of children with disabilities were concerned for their child’s mental health compared with 43% of parents with children without disabilities.
- 76% of parents of children with disabilities were very concerned about regulating their child’s anxiety and emotions, compared with 57% of parents of children without disabilities.
- 58% of parents of children with disabilities or long-term conditions were very concerned for their child’s academic success compared with 36% of parents of children without disabilities.
- 6 in 10 parents of children with disabilities were very concerned about social isolation compared with 5 in 10 parents of children without disabilities.
Diana Gerasimov holds a bachelor’s degree from Concordia University in Communication and Cultural Studies.
Note
- Learn more about the impact of COVID-19 on mental health in Family Finances and Mental Health During the COVID‑19 Pandemic and Do Adults in Couples Have Better Mental Health During the COVID‑19 Pandemic?
COVID-19 IMPACTS: Family Life, Traditions and Rituals
February 26, 2021
While COVID-19 has affected families across Canada and disrupted many of our routines, roles and relationships, it hasn’t stopped family life. Whether we are connecting to celebrate milestones or providing support in difficult times, people are finding diverse and creative ways to keep doing what families do – often with some help from technology.
According to a recent Leger survey,1 some families have taken their family traditions, celebrations and gatherings – both joyous and sad – through video conferencing platforms such as Zoom and Microsoft Teams. While the experience may not be the same as hugging and talking to our loved ones in person, these adaptations are allowing many families to continue to smile, laugh, cry and grieve together. The data show that most, but not all, find them less meaningful than in person but that, for many, it is better than nothing.
COVID-19 IMPACTS: Marriage and weddings
With public health measures restricting in-person gatherings across Canada, many couples in the early months of the pandemic who had planned to get married postponed their wedding plans, but with continuing restrictions on social gatherings, some have gone ahead, “tying the knot” virtually, connecting with their families and friends using video conferencing platforms.
The survey found that…
- In the past year, 7% of respondents had participated in a wedding on a video conferencing platform (e.g. Zoom, Microsoft Teams).
- Those with children in the household (13%) were more than twice as likely as those without children at home (5%) to have participated in an online wedding.
- The likelihood of having participated in an online wedding decreased with age:
- 12% of those aged 18 to 34
- 8% of those aged 35 to 54
- 2% of those aged 55 and older
- Among those who had participated in an online wedding, a slight majority said it was less meaningful than in person; those with children and younger respondents were more likely to report it as more meaningful:
- Slightly over half (54%) said it was less meaningful, and 25% said it was “about the same.” However, 21% found it “more meaningful.”
- Respondents with children in the household (32%) were more than twice as likely than those without children at home (12%) to report it as a more meaningful experience.
- The likelihood of saying it was more meaningful dropped sharply with age:
- 32% of those aged 18 to 34
- 14% of those aged 35 to 54
- 0% of those aged 55 and older
COVID-19 IMPACTS: Grief and loss
Family grieving has also been taking place online, with many families hosting funerals on video conferencing platforms (e.g. Zoom, Microsoft Teams). Respondents in the survey were twice as likely to report having participated in an online funeral (14%) than an online wedding (7%).
- 1 in 7 surveyed Canadians (14%) said they have participated in a funeral on a video conferencing platform in the past year.
- Respondents with children in the household (16%) were more likely than those without children at home (13%) to have participated in an online funeral.
- The likelihood of having participated in an online funeral increased with age:
- 12% of those aged 18 to 34
- 14% of those aged 35 to 54
- 16% of those aged 55 and older
- When those who had attended an online funeral were asked about how meaningful their experience was compared with an in-person funeral:
- More than one-third said it was “about the same” (25%) or “more meaningful” (9%), while the remaining two-thirds (66%) said it was “less meaningful.”
- Respondents with children in the household (14%) were twice as likely as those without children at home (7%) to report it as a more meaningful experience.
- The youngest age group was the most likely to report it being more meaningful:
- 17% of those aged 18 to 34
- 4% of those aged 35 to 54
- 8% of those aged 55 and older
Adaptability and creativity will continue to play an important role in keeping families connected under COVID-19. While this survey showed that families clearly miss their in-person gatherings, these virtual adaptations of weddings, funerals and other family gatherings will likely persist in some format post-COVID (perhaps alongside in-person events), as they allow for family and friends at a distance to stay connected and experience important family events together.
Note
- A survey was conducted by Leger for the Association for Canadian Studies on February 12 and 13, 2021 with 1,535 respondents. While no margin of error can be associated with a non-probability sample, for comparative purposes the national sample of 1,535 Canadians would have a margin of error of ±2.5%, 19 times out of 20.
The Complexity and Impacts of High-Conflict Family Cases
Rachel Birnbaum and Nicholas C. Bala discuss family relationships after high-conflict separations and divorces.
COVID-19 IMPACTS: Couple Relationships in Canada
Ana Fostik explores the family impacts of uncertainty and economic downturn on couple relationships in Canada.
COVID-19 IMPACTS: Youth Well-being in Canada
Edward Ng, PhD, and Nadine Badets
August 27, 2020
Spring and summer 2020 have been a unique time for children and youth in Canada, as families across the country have been adapting their routines, plans and activities in light of physical distancing and other public health measures in place to prevent the spread of COVID-19. With schools closing their doors and moving online in the spring, nearly 5 million children and youth across the country were no longer spending their days near their friends and peers as they and their families adapted and reacted to the evolving situation.1
While surveys have shown that most youth are adhering to public health measures and have demonstrated resilience, this disruption had been difficult for many. In a poll conducted by UNICEF Canada, the toughest aspects cited by youth have been not being able to leave the house, go to school and spend time with friends.2 This matters for the well-being of children and youth, since research shows that social interaction is fundamental in youth development, as positive influences by and among peers are important for students’ academic achievement and success later in life.3
Youth more concerned about family contracting COVID-19 than themselves
While youth have mostly been homebound and self-isolating themselves, some of their immediate family members have continued commuting to work, and therefore risking infection and transmission.
In the COVID-19 Social Impacts Youth Survey conducted in mid-May jointly by the Association for Canadian Studies, Experiences Canada and the Vanier Institute of the Family, nearly 4 in 10 (39%) youth aged 12 to 17 surveyed expressed concerns of contracting COVID-19 themselves,4 compared with more than half (56%) of adults who were surveyed in early May.5 This may be in part due to the current understanding regarding the perceived lower likelihood of experiencing complications and risk with COVID-19 among younger age groups. As well, the same sets of polling data showed that the fear of someone in one’s immediate family catching the virus is higher for both youth and adults (71% and 67%, respectively).
Most youth bored, but also happy, under public health measures and physical distancing
In the same youth survey, more than 80% of youth reported being bored but, interestingly, a similar proportion also reported being happy (89% among youth aged 12 to 14 and 84% among those aged 15 to 17).6 This may be in part due to shifting time use patterns due to school closures. Nearly 7 in 10 of surveyed youth reported they were relaxing more than before the pandemic, with the common activities including watching videos/movies/television or listening to podcasts (78%), spending time on social media (63%), listening to music (59%) and playing electronic games (51%). Youth who reported feeling bored or happy during the pandemic were more likely to report that they spend more time watching videos/movies/television during the pandemic than before it (79% and 81%, respectively).
Technology may be playing a larger role in many people’s lives, but it is not the only way youth are keeping busy. Nearly half (45%) of youth reported helping with chores around the house more than before, while slightly more than one-third of youth were doing arts or crafts (36%) or puzzles (35%) more so than before the pandemic.7
Meanwhile, even before the pandemic, parents had already been expressing concerns about youths’ preoccupation with technology.8, 9 During the lockdown, approximately 64% of the parents who responded to a Statistics Canada crowdsourcing survey were worried about their children’s amount of screen time use.10 According to UNICEF, however, the most robust studies suggest that moderate use of digital technology tends to be positive for children and youths’ mental well-being, while no use or too much use can have a small negative impact.11 Internet and digital technology, while providing a positive source of help and a sense of inclusion, can also open up possibilities of cyber-bullying, impact mental health and exacerbate sleeping problems.12
More than one-third of surveyed youth experienced a negative impact on their mental health
Prior to COVID-19, youth were known to experience higher rates of mental illness and poor mental health than older age groups in Canada. For example, the rate of depression among youth aged 15 to 24 was higher than any other age group.13 A recent study of Canadian Community Health Survey data show that among youth aged 12 to 17, there was a decline of 6% in reporting excellent or very good mental health from 2015 to 2019 (78% and 73%, respectively).14 Further compounding the issue of youth mental health is that, in 2018, suicide was the leading cause of death among male youth aged 15 to 19 and was the second leading cause of death among female youth in Canada.15
In mid-May, more than one-third (37%) of respondents in the youth survey reported that they have experienced negative impacts to their mental health.16 When compared with adults aged 18 and older surveyed in early May,17 youth aged 12 to 17 were more likely to report feeling sad (57% versus 45%, respectively) and irritable (65% and 39%) than adults, and were more likely to report having trouble sleeping (50% versus 35%).
Another survey of youth and young adults aged 14 to 27, conducted April 10 to 14, 2020 for the Centre for Addiction and Mental Health (CAMH), also found a decline in reported mental health early in the pandemic, both for those with pre-existing mental health issues and those without.18
One immediate effect of the mental health repercussions of the pandemic has been an increased demand for mental health and support services for youth. The Kids Help Phone, a 24/7 national support and crisis line for children and youth, saw a jump in the number of calls and texts for help in mid-March 2020, double that of the previous year, with close to 2,000 calls or texts per day.19 The number of crisis calls has also increased, resulting in more interventions by emergency services than usual, with the organization making 8 to 10 calls to emergency services per day since the pandemic started.
Youth spending more meaningful time with their family, but they miss their friends
The shift to working and schooling from home and the disruption of regular routines and schedules have provided families with more opportunities to connect. The youth survey data from mid-May showed that two-thirds (67%) of youth reported having more meaningful conversations with their families during the pandemic than before.20 By comparison, only 50% of surveyed adults in early May reported having meaningful conversations with their spouse or partner.
In terms of family relationships, close to one-quarter of parents reported spending more time with children under lockdown (24%).21 For both youth and adults, the vast majority reported that they are supporting each other well within the family during the lockdown (74% and 81%, respectively). However, around 43% of youth reported arguing more with their families, while only 19% of adults reported arguing with their spouse or partner.
On the other hand, youth are feeling a strong loss of connection to their friends. About 70% of youth reported that they have been homebound during the pandemic, with the exception of going out for necessities, with only 24% reporting that they visited friends and family during the week before the survey.22
According to Angus Reid, youth reported that missing their friends has been the worst part about being stuck at home (54%).23 More than half of youth indicated that the COVID-19 lockdown has had a negative impact on their relationships with friends (53%).24 Statistics Canada’s crowdsourcing survey also provided the parents’ perspective. Almost three-quarters of participating parents (71%) were concerned about their children’s lack of engagements to socialize with friends, and 54% of parents were concerned about their children’s social isolation.25
Distance learning during the COVID-19 pandemic: A painful lesson?
The virtual home school arrangement has been challenging for many families and teachers across Canada. This pandemic-induced online learning has been described as the biggest distance learning experiment in history.26 Amid the abrupt shutdown of schools, teachers had to adjust their teaching styles with little training or resources.
More than half (51%) of youth indicated that the pandemic has had a very negative effect on their school year and/or their academic success.27 Only 27% reported that they “totally agree,” and another 43% partially agreed, that they are doing a good job at getting schoolwork done from home.
About 41% of youth aged 12 to 17 reported missing going to school “a lot,” and another 31% said they “somewhat” missed school. Lack of access to peer/school/academic resources, motivation, time management and online settings make up just some of the challenges of distance learning.28 Though 75% of youth claimed to be keeping up with school while in isolation, many were also unmotivated (60%) and disliked the arrangement (57%) (i.e. online learning and virtual classrooms).29
Distance learning requires Internet access, and while the 2018 Canadian Internet Use Survey found that 94% of Canadians had home Internet access, there nonetheless exist inequities in the ability of school children to actively participate in online education. The reasons among those who did not have Internet access included affordability of the Internet service (28%), equipment (19%) and unavailability of Internet service (8%).30
In addition, while around 8 in 10 youth said they always have enough money to meet their basic needs, such as for food, clothing, health care and housing,31 meeting basic needs and having access to a comfortable study environment at home during the pandemic may be even more difficult for youth and families living with low-income or newly experiencing job and income loss. In addition, closures of schools may impact food security, as some school meal programs were designed to alleviate family food insecurity for those students in low-income situations.32
Long-term monitoring of COVID-19 impacts important for youth well-being
Without school, extra-curricular activities and other opportunities to see peers, youth are missing out on important and valued time for socializing with friends, classmates, teachers, coaches and more – all of which could be fundamental in their scholastic and character development. Although alleviated somewhat through social media, texting, calling and other communication technologies, the mental health of youth in Canada has been greatly impacted during COVID-19.
Previous studies on the impact of school interruptions, such as teachers’ strikes and school closures during the 1916 polio pandemic, have shown short- and long-term negative effects on academic development and knowledge acquisition.33, 34, 35 A recent study on the potential impact of the pandemic on youth education in Canada highlighted that the adverse effect might increase the socioeconomic skills gap by as much as 30%.36 As provincial authorities and school boards consider how to proceed to re-open schools in a safe way to control COVID-19 spread,37 innovation and adaptation in our education system will be important in avoiding or mitigating gaps in academic achievement, now and in the years to come.
Edward Ng, PhD, Vanier Institute on secondment from Statistics Canada
Nadine Badets, Vanier Institute on secondment from Statistics Canada
Notes
- Erin Duffin, “Enrollment in Public Elementary and Secondary Schools in Canada in 2017/18, by Province,” Statista (October 29, 2019). Link: https://bit.ly/311SjPn.
- UNICEF Canada, U-Report Canada: Impacts of the COVID-19 Pandemic on Young People in Canada – Poll 2: Examining the Issues (May 2020). Link: https://bit.ly/2FvZg41 (PDF).
- Shqiponja Telhaj, “Do Social Interactions in the Classroom Improve Academic Attainment?” IZA World of Labor (June 2018). Link: https://bit.ly/3hPqGzR.
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth (May 21, 2020). Link: https://bit.ly/3jlmZn3 (PDF). The Association for Canadian Studies’ COVID-19 Social Impacts Network, in partnership with Experiences Canada and the Vanier Institute of the Family, conducted a nationwide COVID-19 web survey of the 12- to 17-year-old population in Canada April 29–May 5, 2020. A total of 1,191 responses were received, and the probabilistic margin of error was ±3%.
- A survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, conducted May 1–3, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,526 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth.
- Ibid.
- Monica Anderson and Jingjing Jiang, “Teens, Social Media & Technology 2018,” Pew Research Center (May 31, 2018). Link: https://pewrsr.ch/30aWglE (PDF).
- Wesley Sanders et al. “Parental Perceptions of Technology and Technology-Focused Parenting: Associations with Youth Screen Time,” Journal of Applied Developmental Psychology (May–June 2016). Link: https://bit.ly/30gsCeV.
- Statistics Canada, “Impacts of COVID-19 on Canadian Families and Children,” The Daily (July 9, 2020). Link: https://bit.ly/3gIzM0U.
- Daniel Kardefelt-Winther, How Does the Time Children Spend Using Digital Technology Impact Their Mental Well-Being, Social Relationships and Physical Activity? An Evidence-Focused Literature Review, UNICEF (December 2017). Link: https://bit.ly/33b3TKQ (PDF).
- OECD, “Children & Young People’s Mental Health in the Digital Age” (2018). Link: https://bit.ly/3jXBFcg (PDF).
- Leanne Findley, “Depression and Suicidal Ideation among Canadians Aged 15 to 24,” Statistics Canada, Catalogue no. 82-003-X, Health Reports, Vol. 28, no. 1, 3–11, (January 18, 2017). Link: https://bit.ly/3ffdt1A.
- Statistics Canada, “Understanding the Perceived Mental Health of Canadians Prior to the COVID-19 Pandemic,” Canadian Community Health Survey, 2019 (August 6, 2020). Link: https://bit.ly/33VJPwj.
- Statistics Canada, “Table 13-10-0394-01 Leading causes of death, total population, by age group” (Accessed August 13, 2020). Link: https://doi.org/10.25318/1310039401-eng.
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth.
- Association for Canadian Studies. A survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, conducted May 1–3, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,526 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Robert Cribb, “Youth Mental Health Deteriorating Under Pandemic Stresses, New CAMH Study Reveals,” The Star (May 28, 2020). Link: https://bit.ly/3ikLMaf.
- Jeff Semple, “Kids Help Phone Calls for Back Up Amid Record Demand – and Canadians Respond,” Global News (June 28, 2020). Link: https://bit.ly/3gbeDMr.
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth.
- Ibid.
- Ibid.
- Angus Reid Institute, Kids & COVID-19: Canadian Children Are Done with School from Home, Fear Falling Behind, and Miss Their Friends (May 11, 2020). Link: https://bit.ly/3kVRReK.
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth.
- Statistics Canada, “Impacts of COVID-19 on Canadian Families and Children,” The Daily (July 9, 2020). Link: https://bit.ly/3gIzM0U.
- Paul W. Bennett, “This Grand Distance-Learning Experiment’s Lessons Go Well Beyond What the Students Are Learning,” CBC News (May 11, 2020). Link: https://bit.ly/33bNEgo.
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth.
- UNICEF Canada, U-Report Canada: Impacts of the COVID-19 Pandemic on Young People in Canada (May 2020). Link: https://bit.ly/2CUd9Z9 (PDF).
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth.
- Statistics Canada, “Canadian Internet Use Survey,” The Daily (October 29, 2019). Link: https://bit.ly/3hWlwSN.
- Association for Canadian Studies, Social Impacts of COVID-19 on Canadian Youth.
- Canadian Medical Association Journal, “Indirect Adverse Effects of COVID-19 on Children and Youth’s Mental, Physical Health,” EurekAlert (June 25, 2020). Link: https://bit.ly/2BWMvOr.
- Michael Baker, “Industrial Actions in Schools: Strikes and Student Achievement,” Canadian Journal of Economics (March 2011). Link: https://bit.ly/3gaona6.
- Michèle Belot and Dinand Webbink, “Do Teacher Strikes Harm Educational Attainment of Students?” (2010) Labour Economics 24(4): 391–406. Link: https://bit.ly/3aYuJI3.
- Keith Meyers and Melissa A. Thomasson, “Paralyzed by Panic: Measuring the Effect of School Closures During the 1916 Polio Pandemic on Educational Attainment,” NBER Working Paper Series 23890 (September 2017). Link: https://bit.ly/3hSzswU (PDF).
- Catherine Haeck and Pierre Lefebvre, “Pandemic School Closures May Increase Inequality in Test Scores,” Research Group on Human Capital Working Paper Series (June 2020). Link: https://bit.ly/30elgbN (PDF).
- Carly Weeks, “Rising Rates of COVID-19 in Children, Adolescents Spark Concerns About Back to School Plans,” The Globe and Mail (June 23, 2020). Link: https://tgam.ca/3hTmFuk.
In Conversation: Katherine Arnup on Death, Dying and Dignity During COVID-19
Gaby Novoa
August 4, 2020
In May 2018, the Vanier Institute published Family Perspectives: Death and Dying in Canada1 by Katherine Arnup, PhD, which examined the evolution of death and dying across generations, the desires and realities of families surrounding death and dying, the role of families in end-of-life care and its impact on family well-being.
With the current conversation surrounding COVID-19 and post-pandemic context, we joined in conversation with Dr. Arnup to hear her reflections on some of the themes explored in the 2018 report, and on the impact of the pandemic on conversations surrounding death and dying in Canada.
Tell us about how you feel COVID-19 has impacted the conversation and attitudes on death and dying among families and policymakers in Canada.
Death is in many ways in the public eye more now than it was prior to COVID-19, and has been from the get-go, once the virus became a presence in the world, because a number of countries experienced a large number of deaths before it really hit here. People were very aware that something major was happening in terms of death.
In Canada, we’ve had daily deaths, casualties and case counts being reported, much like in wartime. There’s been war imagery accompanying this in many ways, but certainly in my lifetime, I’ve never seen anything like this – it’s almost unavoidable. If you visit the CBC website, the first thing you see is the current counts, which makes you very aware of how many people have died. You can’t really get away from it, with these constant reminders. There’s a sense that we’re “at war” with a virus. Especially at the beginning, there was a sense that it could be anywhere, people nearby could be carrying it, and you could get it and it could kill you. A lot of fear – fear of the virus and a fear of dying.
One of the themes in Family Perspectives: Death and Dying in Canada is that people’s fear of death and dying deters families from having important conversations about it. Do you think the pandemic has forced people to think about death in a more in-depth way, or have anxieties and fears caused more avoidance of the conversation on death and dying?
I think it’s the latter. In my report, I was talking about a kind of acceptance of death and planning for death. But since there are many unknowns around COVID, which has struck so many people throughout the world, it’s different from anything any of us have experienced.
I think one of the biggest ways that COVID-19 and death have been front and centre throughout the pandemic is around seniors and their families. It’s quite true that the virus poses a greater risk for seniors than for anyone else, although certainly other factors make people vulnerable as well. However, seniors, and particularly people in their 80s and 90s and people with comorbidities, are likely to have a bad result and perhaps die as a result of contracting the coronavirus.
That’s especially been the case in long-term care facilities. In Ontario, the long-term care facility in Bobcaygeon was one of the first ones that the public really became aware of, where they had many deaths in a short period of time. Overall in Canada, the most recent data on this showed that 81% of the deaths in Canada were in long-term care, compared with the average of 42% in developed countries in the OECD.2 The numbers are much higher in Canada, so dramatic that the military was called in for assistance in Ontario and Quebec, which also fits with the military and war metaphors. They reported incredibly appalling conditions in those long-term care homes.3
I think a lot about long-term care homes now in a way that I didn’t before. I believe that I was just like most Canadians in that I didn’t think about them, beyond saying “I hope I never end up there,” and I think that’s very typical of Canadians. Maybe true for people in other countries, but I can say it for Canadians and that fits in with some of the things I’ve written about in the 2018 report and elsewhere: we want to live forever, but we want to be healthy, strong and independent – those are huge values for us.
Living in long-term care is something we really don’t want to think about, so most of us haven’t looked at the conditions there – many of which existed before the pandemic. That is, often four people to a room, staff working at several homes, understaffing, staff being very busy rushing from patient to patient and then going to another home. A lot of those things were happening already, and they created the conditions for the pandemic to grab hold and decimate long-term care populations.
I think those who have family in long-term care homes have had a huge wake-up call. They probably knew something about the conditions, and some of them were active caregivers in those homes – that is, going and caring for their loved ones – while some people virtually never visited. My aunt was in a long-term care home in a small town not that far from Bobcaygeon. I visited her when she was dying, and was actually really impressed with that home. She had her own room and you could tell that the staff cared for their patients, for their residents. I don’t think everything negative that we’ve seen is the case for all long term-care by any means. But we mostly just haven’t thought about it.
Pat Armstrong, a major scholar of health care in Canada, has been involved in a 10-year study of long-term care homes.4 She and her team remind people that though we don’t want to think about them, any of us could end up in long-term care almost in the blink of an eye: a major accident or a stroke, a fall that means we can’t care for ourselves, a diagnosis of dementia. Any of those things could mean that I end up in a long-term care home. I don’t want to, like most people, but we always think it’s going to be somebody else and not us. I think that the crisis has made us aware that it can be anyone – our mothers, our fathers, our sisters, ourselves. With change – and only one changed circumstance has to happen – we could be there as well. It’s a reminder that we all need to be fighting to change those institutions and how people die.
I was looking at the list of desires and assumptions discussed in the report, two of which stood out as I read the military report: we want to die at home and we want to die with dignity. It’s very clear that there was no dignity in the way that people were dying in long-term care homes. Indeed, there was no dignity in how they were being cared for, because of the conditions there. It’s also clear that people are there in those facilities because families can’t take care of them. It’s not that families don’t care. It’s that their own lives and the demands of their lives, and the lack of home care, means that they can’t care long-term for a family member who’s got dementia and maybe is acting out, or a family member who really needs 24/7 care.
Many Canadians also assume that they can get all the home care they and their families need. The pandemic has meant that many people had to cancel the home care that was coming in, especially at the beginning, because they were afraid to get COVID from their home care provider. Home care providers, by their very nature, are usually working in several homes. So, they’re potentially carrying the virus to many homes. It’s meant that not only is there not enough home care generally, but in the case of COVID, people were also hesitant to have those carers coming into their homes.
Like the pre-existing challenges in many long-term care homes, we’ve seen certain vulnerabilities and inequities amplified within the pandemic. Do you find any hope in how the conditions of long-term care are now being brought to greater public awareness?
With long-term care homes, I feel a need to speak out about it, and to press governments to make changes that could have a huge impact, such as federal standards, or for senior care to be included in the Canada Health Act so that it becomes a shared responsibility across governments.
I think families have really mobilized and have seen the shortcomings and some of the reasons why the conditions are so bad. This is partly due to the for-profit homes, which have higher deaths, but also a lack of inspections and of enforcement of what exists in the law. In bringing it to the public attention as it has, in being such a tragedy, I think that there is hope for improvement, and I hope that many more people are now aware that it could be them, that it could be their families.
People who have children with severe disabilities who are living in congregate care are also facing similar issues of not being able to have family with them, as they still aren’t able to go into those homes. I do see a lot more discussion now around families as caregivers, having them recognized as caregivers and not just as visitors, as they’re being talked about. It’s an issue that the Vanier Institute has raised, I’ve done work with the Change Foundation, and there are other organizations that have made progress on that. So, I feel positive and see hope there for a recognition of the role of caregivers and their importance in the health and well-being of those who are cared for.
There has been increased opportunity to talk about advanced care directives. Even if people aren’t necessarily having those conversations, I think that if they’re faced with a family member getting COVID, it will spur the realization that we don’t always know what our family member wants. Even though the conversation around death hasn’t come on to the table in the best way, I think it provides openings for those of us who have been promoting the importance of advanced care. It provides an avenue for discussion, to be able to say to people that this is a realistic concern. We just never know when something will happen, and something will happen. We need to know what each other wants. Our children need to know what we want – I think the pandemic opens the door to that.
I’m writing and have been making videos, and I will be encouraging people in one of my next ones to talk to their family members (if they haven’t already) about what they want and about making advanced care directives, because it’s really important. Family members having to say “I just don’t know what Mom would want” is a mistake that doesn’t have to happen.
I feel optimistic about these things, and optimism in the face of a pandemic is in short supply. I’m optimistic around that sense that we’re all in this together, which we began this pandemic with. Our Prime Minister stressed this idea every day in his talks, and other people did as well. I think there has been significant pulling together around a sense of community and caring for one another. I’ve experienced this in my own neighbourhood – people who never normally talked to one another are checking in. When you go for a walk, people ask how you are doing and it’s genuine. I think that’s a strangely positive thing that is a result of the pandemic. I hope that it lasts, that people are doing things for elderly neighbours and that they’re more aware of who might be in need of help on their street. Anything that increases a sense of community I think is a great thing.
You touch on this point in your video “Expanding Our ‘Bubbles,’”5 on feeling reassured in many ways by this sentiment that we’re all in this together, though you also note that it has become increasingly apparent that we’re not all in the same boat. We might all be in it together, but the way we’re experiencing it varies greatly, whether it’s higher risk among seniors and other groups.6 Could you elaborate?
When you look at the breakdown of the areas that are still COVID hotspots, it’s where there are people living in poverty, people of colour, people who are working high-risk jobs in health care and in the service sector, and people living in large numbers together because they might not be able to afford anything else. Significant outbreaks among migrant workers employed in agricultural work and workers in food processing plants also demonstrate the impact of inequalities in our society on people’s vulnerability in the pandemic.
Another important way in which people haven’t been in it all together has been in families’ inability to have funerals, wakes, services or celebrations of life during the pandemic. I think this is having a huge impact on those who aren’t able to mark the death of a loved one with friends and family. There have been many families who couldn’t have a service of any kind, who couldn’t hug, who couldn’t get together beyond small groups. I just wonder what happens to that grief.
Many of those people who died, died alone. People in long-term care facilities and in hospitals have died alone. None of us wants that to happen. None of us wants it to happen to the people we love, and we don’t want to have it happen to us. It is an important tenet of hospice palliative care: let no one die alone. That this has been happening on a huge scale for the families left behind, it means enormous grief and guilt, feeling that “I couldn’t be there for Mom” or “I couldn’t be there with Mom when she was dying.” That’s heartbreaking. I don’t know what people do with that; you kind of have to push it down. I think about how all the obituaries say, “When it’s possible, we’ll have a service.” It’s hard for me to imagine all those services and where they’ll happen and whether that will provide the closure and support that people need. I certainly haven’t seen anything like that in my lifetime.
What gives you hope going forward?
I think about these questions: What do we want when we die? But also, what do we want as we grow older? What do we need to support us in that? How are we dealing, in general, with aging and dementia? What do we hope for? How can we create places that are very different from long-term care homes? How can we make that happen?
Katherine Arnup, PhD, is a writer, speaker and life coach specializing in transitions, and a retired Carleton University professor. Author of Family Perspectives: Death and Dying in Canada (and several books, including “I Don’t Have Time for This!”: A Compassionate Guide to Caring for Your Parents and Yourself and Education for Motherhood, she has pioneered studies on family experiences and provided unique insights into family life throughout her career.
Gaby Novoa is responsible for Communications at the Vanier Institute of the Family.
This interview has been edited for length, flow and clarity.
Notes
- Katherine Arnup, PhD, Family Perspectives: Death and Dying in Canada, The Vanier Institute of the Family (May 2018).
- Canadian Institute for Health Information, “Pandemic Experience in the Long-Term Care Sector: How Does Canada Compare with Other Countries?” CIHI (June 25, 2020). Link: https://bit.ly/3hGl4bc.
- Canadian Armed Forces, “Op LASER – JTFC Observations in Long Term Care Facilities in Ontario,” CAF (May 20, 2020). Link: https://bit.ly/2CJPnit.
- Pat Armstrong is a Distinguished Research Professor in Sociology at York University and a Fellow of the Royal Society of Canada. Link: https://bit.ly/3g3XSDn.
- Katherine Arnup, “Expanding Our ‘Bubbles,’” (YouTube). Link: https://bit.ly/2X15sqE.
- In Family Perspectives: Death and Dying in Canada, Arnup writes that experiences of death and dying are affected by factors of gender, race, class, ethnicity, geography, marginalized status, ability, sexual and gender identity, marital status and Indigenous, First Nation, Inuit and Métis status.
Families in Canada Adapting: My Family’s COVID Journey
While COVID-19 has affected families across Canada and the social, economic, cultural and environmental contexts that impact their well-being, it hasn’t stopped family life by any means. Whether it’s managing work–family responsibilities, connecting to celebrate milestones or providing support in difficult times, people are finding diverse and creative ways to keep doing what families do.
As families in Canada continue to manage these transitions, the Vanier Institute is gathering, compiling and sharing these “stories behind the statistics” to provide insights and into family strengths, resilience and diverse experiences across the country.
Edward Ng, PhD
(July 23, 2020) March 16, 2020 ended up being not just another Monday. While this was the first official day of spring break for public school students in Ontario, the school board suddenly announced that the break would be instead two weeks, which was later extended until further notice. Inadvertently, some 2 million Ontario public school students – including my younger daughter, who is in Grade 9 – started a long journey of distance learning from home as a result of the pandemic.
Family home suddenly becomes school and shared workspace
The night before, I had also been asked not to report to work at my office near downtown Ottawa due to public health measures aimed at preventing the spread of the coronavirus. At the same time, my older daughter, a university student, was told that classes would move online, as the campus began to shut down.
Among my family of four, only my wife continued to leave home for work. However, after a case of COVID-19 was reported at her workplace in late March, everyone was then asked to work from home from then on, a decision that would have been unimaginable before the pandemic began. I began to wonder if this was the beginning of the end of an office-centric era, with huge implications for work and family.
Though we have an Internet connection, our home setting is not equipped to be a home office and/or a home school. Since my wife works in a sector dealing with clients over the phone, I quickly rearranged a room to set up a temporary office for her. My younger daughter, after an extended spring break, soon started to receive daily instruction and lessons from her teachers online, which meant all four of us were now using a single Internet connection almost constantly. Ultimately, we’ve had to contact our Internet service provider to upgrade our hardware, which mitigated our problems and frustrations – and the demand for me to become an Internet technologist!
Reflecting on experiences and emotions through music
In May, two months into the lockdown, my daughter was asked by her Grade 9 music teacher to select some songs that reflected her emotional state while learning from home. She chose “Stayin’ Alive” by the Bee Gees. I was surprised since she is not of the era of the Bees Gees, who were famous in my birthplace of Hong Kong when I was growing up. This upbeat disco hit of the late 1970s was described by one of the songwriters as actually being rather serious in its focus – it is about survival1 when life is “goin’ nowhere.”
Life goin’ nowhere, somebody help me
Somebody help me, yeah
Life goin’ nowhere, somebody help me, yeah
I’m stayin’ alive
It’s a cry for survival that resonated with my daughter’s experiences during the COVID-19 pandemic, with her feelings and concerns regarding the virus amplified as a visible minority2 teen.3 I admired her perseverance as she avoided venturing out as much as possible throughout the lockdown. But she also felt hopeful: the second song she chose was “Let’s Go Fly a Kite” from Mary Poppins, reflecting her anticipation of going out without fearing COVID-19.
Care and concern across generations
Like the majority of Canadians, I am more concerned about my family contracting COVID-19 than myself, and surveys have consistently shown that visible minorities experience both of these concerns at higher rates than those who are not visible minorities.4, 5 Like many families, my care and concerns extend across generations, to older and younger generations.
My university-aged daughter works as a part-time cashier at a neighbourhood pharmacy. Each shift, she ventures out to her essential job, and we were concerned about the risk of being infected with COVID-19 through her exposure to customers. In mid-April, she came down with a fever and dry cough, which are some of the possible symptoms. We were worried, and encouraged her to self-isolate by taking a leave of absence to ensure she was not positive. As soon her symptoms subsided, she returned to work, only to find her workplace had been transformed, with plexiglass installed at the cash to minimize the risk of infection. One time, she reported a scary moment when a client, while paying for the purchase, kept on coughing at the plexiglass without any concern for others!
For about three years, my mother-in-law has been staying in a long-term care home in Toronto, and we visited her whenever we went to the city. Given that these care homes in Ontario and Quebec have become the epicentre for COVID-19, we became very nervous for her. In fact, we found out that a resident at her care home was tested positive in mid-May, which indicated an outbreak, according to the local public health authority. Further investigation was conducted of staff and residents, with encouraging results that contradicted the original findings. We were relieved when the Public Health Authority withdrew its order of outbreak for the facility.
With the Ontario ruling that no visitations were allowed at these care homes at the early stage of the pandemic, we could only use online communication, such as Skype, to stay connected through virtual visits. The workers there at the care home have told us that the residents there have been bored during the pandemic and welcome these virtual visits. Now that Ontario is starting to allow visitors into nursing homes, we are making plans for a physical visit, which still needs to respect social distancing protocol.
Care and concern across borders
I experienced concerns for my family prior to the declaration of the COVID-19 pandemic. Back in February, my relatives who were visiting from East Asia decided to leave Toronto to return home to Hong Kong before Air Canada cancelled all direct flights. During that time, COVID-19 was affecting that part of Asia severely and I had suggested they stay longer in Toronto, but they decided to go. To soothe my own worry, I searched around and managed to purchase some non-surgical masks for them to use in Hong Kong. (Note that, at that time, in mid to late-February, face masks were hard to find for purchase, even in Ontario.)
In hindsight, however, my relatives felt that they had made the right decision to leave, as COVID-19 cases began to increase in Toronto and as airports started to close in Canada. Interestingly, they are now back in Toronto for their annual summer visit to Canada, just as a COVID-19 outbreak is occurring in Hong Kong.
Perhaps due to my close connection to Asia, I was quite concerned about COVID-19 before it became a household name in Canada. I vividly recall how SARS (Severe Acute Respiratory Syndrome)6 hit my homeland as well as Toronto in 2003. So, as early as February of this year, near the beginning of the outbreak in Asia, I had closely followed the development of this emerging virus, which was impacting families all around the world.
Time for family memories and conversations
Thinking of the song “Let’s Go Fly a Kite” brings back memories of when my daughters were young, when we would often do this together in a nearby park.7 We would spend a lot of time talking and laughing together, and once the kite caught the wind, we would follow along and enjoy watching it soar into the sky.
As they have grown to become more independent over the years, and I focused on my own work and other involvements, there are usually few opportunities for these kinds of moments. But the pandemic has reminded me to spend time with them – and provided some opportunities to do so – before they graduate onto the next stage of life. Thankfully, the “lockdown” has allowed us time, as a family, to have some meaningful discussion about matters important to life. For that, I am thankful.
Edward Ng, PhD, is an analyst at the Vanier Institute of the Family.
Notes
- Interestingly, “Stayin’ Alive” has been used to train medical professionals to provide the right number of chest compressions per minute while performing CPR, since its tempo of close to 104 beats per minute falls within the recommended 100–120 chest compressions per minute recommended by the British Heart Foundation while performing the life-saving procedure.
- “Visible minority” refers to whether a person belongs to a visible minority group as defined by the Employment Equity Act and, if so, the visible minority group to which the person belongs. The Employment Equity Act defines visible minorities as “persons, other than Aboriginal peoples, who are non-Caucasian in race or non-white in colour.” Categories in the visible minority variable include South Asian, Chinese, Black, Filipino, Latin American, Arab, Southeast Asian, West Asian, Korean, Japanese, Visible minority (i.e. “not included elsewhere”), Multiple visible minorities and Not a visible minority. According to the 2016 Census of Canada, close to 70% of the visible minorities are born outside Canada (69%).
- According to a survey by the Vanier Institute of the Family, the Association for Canadian Studies and Experiences Canada conducted from April 29 to May 5, 2020, more than half (52%) of visible minority youth said they were somewhat or very afraid of catching COVID-19, compared with 34% of those who are not visible minorities. Link: https://bit.ly/3jlmZn3.
- More than 6 in 10 surveyed visible minorities (62%) said they were afraid of contracting COVID-19, but 73% were even more fearful for family members to get the virus, compared with 54% and 66%, respectively, among those who are not visible minorities.
- A survey by the Vanier Institute of the Family, the Association of Canadian Studies and Leger, conducted May 1–3, 2020, included 1,526 Canadians 18 years of age or older, randomly recruited from LEO’s online panel. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (Web panel, in this case). However, for comparative purposes, a probability sample of 1,526 respondents would have a margin of error of ±2.51%, 19 times out of 20.
- Severe acute respiratory (SARS) is a respiratory disease caused by severe acute respiratory syndrome coronavirus (SARS-CoV or SARS-CoV-1), which resulted in approximately 300 deaths in Hong Kong and more than 40 deaths in Canada during the 2002–2004 SARS outbreak.
- “Let’s Go Fly a Kite” is from the Walt Disney classic Mary Poppins, featured at the end of the film when George Banks (played by David Tomlinson), realizes that his family is more important than his job, and decides to take his family on a kite-flying outing.
Published on July 23, 2020
COVID-19 IMPACTS: Families and Housing in Canada
Nadine Badets, Gaby Novoa and Nathan Battams
July 21, 2020
The COVID-19 pandemic has impacted families and family life across Canada, with economic lockdowns and physical distancing measures affecting the social, economic and environmental contexts associated with family well-being. Housing is no exception: prospective homebuyers are seeing a real estate cooling down in the face of uncertainty, while physical distancing measures are not easily actionable for many families living in crowded or unsuitable housing.
The COVID-19 lockdown has considerably slowed Canada’s real estate market
Most major cities in Canada (16 of 27) had little or no change to new housing prices in April 2020. However, sales of new homes and resales of older homes across Canada all declined significantly during the height of the pandemic. Builders surveyed by Statistics Canada in April 2020 reported a decline of almost two-thirds (64%) in sales of new homes when compared with the same month in 2019. The Canadian Real Estate Association reported a 58% decline in home resales in April, year over year.1
In light of the closure of economies and significant loss of jobs, the provinces and territories have issued eviction bans and payment suspensions to support renters. The Canada Housing and Mortgage Corporation (CMHC) has also urged all landlords, including those with CMHC insurance or financing, to abstain from evicting renters during the COVID-19 pandemic.2 However, as the pandemic restrictions begin to lift, many people and families in Canada could be faced with evictions and/or owing large amounts of money for missed rent.
Demand for homeless shelters increased dramatically during lockdown
Prior to the COVID-19 pandemic, challenges with housing accessibility and affordability was unequally and excessively prevalent among certain groups within Canada, including newcomers and refugees, racialized groups, LGBTQ2S people, seniors, Indigenous peoples and persons with disabilities and/or mental health conditions.3
Homelessness4 is particularly concerning during the pandemic, as it exposes people to unsafe living conditions with severe consequences for physical and mental health, and makes it challenging to abide by new public health orders such as physical distancing.
Whether people are moving from home to home (often referred to as “hidden homelessness”), spending time in shelters,5 living transiently and sleeping in various places, or a combination of these, those experiencing homelessness are often in close proximity with multiple people and with little to no access to the necessary resources for recommended hygiene practices.6
In 2014, it was estimated that at least 235,000 people in Canada experience homelessness in a given year and around 35,000 are homeless on a given night. Individuals usually spend an average of 10 days in shelters, and families usually spend twice that amount of time.7 Throughout the COVID-19 pandemic, shelters in Canadian cities have reported increased use by new and familiar clients;8 however, due to physical distancing restrictions, shelters have had to drastically reduce the number of beds and spaces they offer, which has left many without a place to stay.9, 10
Increases in reports of domestic violence,11 abuse12 and mental health concerns13 have also left many individuals and families with no place to stay. Many shelters have increased support to the homeless by creating spaces in community centres, hotels and permanent housing, though they lack the financial capacity to meet the increased demand for shelter services.14, 15
Housing issues in First Nations and Inuit communities are related to increased COVID-19 risk
Since the COVID-19 pandemic started, Indigenous leaders and peoples have been calling attention to the continuing devastation from tuberculosis in First Nations and Inuit and communities, reminding Canada that COVID-19 is not the only pandemic they are facing.16, 17
In 2017, Inuit had a rate of 205.8 cases of tuberculosis per 100,000 people, and First Nations (on reserve) had 21.7 cases per 100,000. Tuberculosis was also high among immigrants, with a rate of 14.7 among those born outside of Canada, whereas for Canadian-born non-Indigenous people the rate was 0.5 per 100,000.18 As of April 19, 2020, the only Inuit region to report COVID-19 cases is Nunavik, with 14 cases (5 recovered and 9 active).19 Among First Nations, data collected through communities show that, as of May 10, 2020, there were 465 cases of COVID-19 and 7 deaths.20
In 2016, Inuit living in Inuit Nunangat21 (the Inuit homeland) were more likely to live in crowded households22 (52%) and in homes in need of major repairs23 (32%).24 Unsuitable housing is also prevalent in some First Nations, where issues such as household crowding (27%)25, 26 and homes in need of major repairs (24%)27 are much higher than for non-Indigenous people in Canada (9% and 6%).28
Household crowding aggravates the risk of catching infectious respiratory diseases like tuberculosis and COVID-19, the latter of which is considered to be even more contagious than tuberculosis.29 Poor housing conditions have been directly associated to quality of health and well-being, with studies showing increased risk of the spread of infectious and respiratory diseases, chronic illness, injuries, poor nutrition, violence and mental disorders.30 Household crowding also complicates – and potentially negates – physical distancing and the isolation of sick people within a household. Homes in need of major repairs can pose health hazards in a variety of ways. In particular, the ongoing lack of sufficient access to water infrastructure in some First Nations poses additional risks of infection and transmission.
Multigenerational households face more obstacles to physical distancing
Multigenerational households are an important part of many families in Canada, as they can facilitate care and support between generations and allow some parents to save money on child care, and facilitate intergenerational learning.31 Between 2001 and 2016, multigenerational households were the fastest-growing household type in Canada, increasing by 38% to reach nearly 404,000 homes.32
These types of households may face unique barriers to social distancing, taking into account the seniors within the home who are considered among the populations most vulnerable to the virus.33
In 2016, 11% of immigrants lived in multigenerational households,34 as did 5% of non-immigrants.35 Indigenous children aged 0 to 14 years were often more likely to live in multigenerational households36 with 13% of First Nations children, 13% of Inuit children and 7% of Métis children, than non-Indigenous children (8%).37
Sustainable Development is intertwined with housing
The COVID-19 pandemic has affected many aspects of housing in Canada, and intensified pre-existing inequalities among marginalized communities across the country. As Canada has committed to the implementation of the UN Sustainable Development Goals, which address factors such as poverty (SDG 1), health and well-being (SDG 3) and reduced inequalities (SDG 10), housing will be an important component of policy responses and conversations on this topic, which is of particular importance in the context of the COVID-19 pandemic.
Nadine Badets, Vanier Institute on secondment from Statistics Canada
Gaby Novoa is responsible for Communications at the Vanier Institute of the Family.
Nathan Battams is Communications Manager at the Vanier Institute of the Family.
Notes
- Statistics Canada, “New Housing Price Index, April 2020,” The Daily (May 21, 2020). Link: https://bit.ly/3d5as2O.
- Canada Mortgage and Housing Corporation, “COVID-19: Eviction Bans and Suspensions to Support Renters: The Latest Updates on Eviction Moratoriums Related to COVID-19” (March 25, 2020). Link: https://bit.ly/3i3ak7R.
- Homeless Hub, “Racialized Communities” (n.d.). Link: https://bit.ly/32b50JX.
- Homelessness can be described as being very short-term (being unhoused for a night or so), episodic (moving in and out of homelessness) or chronic (long-term). For more information, see the Homeless Hub website. Link: https://bit.ly/2CuWgDK.
- Shelters include emergency homeless shelters, violence against women shelters and temporary institutional accommodations. For more information, see the Homeless Hub website. Link: https://bit.ly/2CuWgDK.
- Jennifer Ferreira, “The Toll COVID-19 Is Taking on Canada’s Homeless,” CTV News (May 22, 2020). Link: https://bit.ly/2N7AcB8.
- Stephen Gaetz, Erin Dej, Tim Richter and Melanie Redman, “The State of Homelessness in Canada 2016,” Canadian Observatory on Homelessness, Canadian Alliance to End Homelessness (2016). Link: https://bit.ly/2zKUsW1 (PDF).
- Ferreira, “The Toll COVID-19 Is Taking on Canada’s Homeless.”
- Nicole Mortillaro, “‘It’s Heartbreaking’: Homeless During Pandemic Left Out in the Cold – Figuratively and Literally,” CBC News (April 17, 2020). Link: https://bit.ly/2NcOQao.
- Matthew Bingley, “Coronavirus: Toronto Officials Call for Provincial Pandemic Plan for Shelters to Avoid ‘Mass Outbreaks,’” Global News (April 20, 2020). Link: https://bit.ly/3dhnWII.
- Cec Haire, “Increase in Domestic Violence Calls Persists Throughout Pandemic, Says Non-Profit,” CBC News (July 2, 2020). Link: https://bit.ly/32eJp3p.
- Public Health Ontario, “Rapid Review: Negative Impacts of Community-Based Public Health Measures During a Pandemic (e.g., COVID‑19) on Children and Families” (2020). Link: https://bit.ly/307gxY8 (PDF).
- Aisha Malik, “CAMH Expands Virtual Mental Health Services Amid COVID-19 Pandemic,” MobileSyrup (May 4, 2020). Link: https://bit.ly/3gVt73i.
- Mortillaro, “‘It’s Heartbreaking’: Homeless During Pandemic Left Out in the Cold – Figuratively and Literally.”
- Ferreira, “The Toll COVID-19 Is Taking on Canada’s Homeless.”
- Olivia Stefanovich, “COVID-19 Shouldn’t Overshadow Ongoing Fight Against TB, Inuit Leaders Say,” CBC News (April 12, 2020). Link: https://bit.ly/3doVTr3.
- John Borrows and Constance MacIntosh, “Indigenous Communities Are Vulnerable in Times of Pandemic. We Must Not Ignore Them,” The Globe and Mail (updated March 21, 2020). Link: https://tgam.ca/2YYhTDY.
- M. LaFreniere, H. Hussain, N. He and M. McGuire, “Tuberculosis in Canada, 2017,” Canada Communicable Disease Report (February 7, 2019). Link: https://bit.ly/2CrvRq9.
- Nunavik Regional Board of Health and Social Services, “COVID-19: 14th CONFIRMED CASE IN NUNAVIK,” News Release (April 19, 2020). Link: https://bit.ly/2OnScIb (PDF).
- Courtney Skye, “Colonialism of the Curve: Indigenous Communities and Bad Covid Data,” Yellowhead Institute (May 12, 2020). Link: https://bit.ly/37W5kgi.
- Inuit Nunangat is composed of four Inuit regions: Nunatsiavut (Northern Labrador), Nunavik (Northern Quebec), Nunavut and the Inuvialuit Settlement Region (Northern Northwest Territories). Inuit Tapiriit Kanatami, “Inuit Nunangat Map” (updated April 4, 2019). Link: https://bit.ly/2WgN4de.
- Statistics Canada (2016 Census of Population) calculates crowded households as an indicator of the level of crowding in a private dwelling. It is calculated by dividing the number of persons in the household by the number of rooms in the dwelling, and dwellings with more than one person per room are considered to be crowded. Statistics Canada, “Persons per Room,” Dictionary, Census of Population, 2016 (May 3, 2017). Link: https://bit.ly/2AZDJyT.
- Major repairs are defined by Statistics Canada (2016 Census of Population) as including defective plumbing or electrical wiring, and dwellings needing structural repairs to walls, floors or ceilings. Statistics Canada, “Dwelling Condition,” Dictionary, Census of Population, 2016 (May 3, 2017). Link: https://bit.ly/3erBnam.
- Thomas Anderson, “The Housing Conditions of Aboriginal People in Canada,” Census in Brief (October 25, 2017). Link: https://bit.ly/316qpmR.
- Ibid.
- Statistics Canada, “Housing Conditions,” Aboriginal Statistics at a Glance: 2nd Edition (December 24, 2015). Link: https://bit.ly/37Ue8ne.
- Anderson, “The Housing Conditions of Aboriginal People in Canada.”
- Vanier Institute of the Family, “Indigenous Families in Canada,” Facts and Stats (June 2018).
- Olivia Stefanovich, “COVID-19 Shouldn’t Overshadow Ongoing Fight Against TB, Inuit Leaders Say.”
- Housing as a Social Determinant of First Nations, Inuit and Métis Health” (2017). Link: https://bit.ly/2DoQ3JV (PDF).
- Asfia Yassir, “Having Grandparents at Home Is a Blessing,” South Asian Post (March 4, 2018). Link: https://bit.ly/2WhlrR5.
- The Vanier Institute, “2016 Census Release Highlights Family Diversity in Canada” (October 25, 2017).
- Caroline Alphonso and Xiao Xu, “Multigenerational Households Face Unique Challenges in Battling Spread of Coronavirus,” The Globe and Mail (March 21, 2020). Link: https://tgam.ca/2O9ss24.
- Defined by Statistics Canada (2016 Census of Population) as households where there is at least one person living with a child and a grandchild.
- Statistics Canada, “Admission Category and Applicant Type (47), Immigrant Status and Period of Immigration (11B), Age (7A), Sex (3) and Selected Demographic, Cultural, Labour Force and Educational Characteristics (825) for the Population in Private Households of Canada, Provinces and Territories and Census Metropolitan Areas, 2016 Census – 25% Sample Data,” Data Tables, 2016 Census (updated June 17, 2019). Link: https://bit.ly/312VGHv.
- Defined as living in a household with at least one parent and one grandparent.
- Statistics Canada, “Family Characteristics of Children Including Presence of Grandparents (10), Aboriginal Identity (9), Registered or Treaty Indian Status (3), Age (4B) and Sex (3) for the Population Aged 0 to 14 Years in Private Households of Canada, Provinces and Territories, Census Metropolitan Areas and Census Agglomerations, 2016 Census – 25% Sample Data,” Data Tables, 2016 Census (updated June 17, 2019). Link: https://bit.ly/3184yvh.
Getting Out, Getting Active and Family Well‑Being
Gaby Novoa and Nathan Battams
June 22, 2020
Summer 2020 will be a unique one for families, as communities across Canada cautiously continue to relax public health measures and restrictions and families manage major transitions at home, at work and in their communities.
Many parents are working from home for the first time, which can present some challenges but also opportunities to spend more time with their children and to foster healthy physical activity behaviours, which, after months of being in physical isolation, will likely be a welcome pursuit for many.
Families are shifting summer plans to manage uncertainties
People typically make family decisions based on choice and circumstance, and the coronavirus pandemic and public health measures have had an impact on both. Responding to a variety of factors related to the pandemic – including financial insecurity, a need or desire to remain close to manage work and family, some continued mobility restrictions and uncertainty whether restrictions will return – it’s not surprising that nearly 6 in 10 (59%) parents surveyed in late April reported that they have changed their vacation plans due to the pandemic, and 72% say that it’s unlikely that they will take a holiday this year.
Children and youth will also be adapting their plans and activities, as many summer camps and organized sports or activities will either be postponed or not taking place. While some organizations are set or pending announcements to open, the impact of the pandemic on family finances may deter some parents from registration in order to carefully manage expenses. Others may avoid sending their kids anywhere due to health concerns or anxiety, particularly if their children live with any immunodeficiency.
With more families spending time at home this summer and plans being changed and adapted, there are growing opportunities for many families to get outdoors and be active together.
Family support critical to children’s levels of physical activity
The newly released Family Influence: The 2020 ParticipACTION Report Card on Physical Activity for Children and Youth reports that less than 1 in 5 children and youth in Canada meet national guidelines for physical activity, sedentary and sleep behaviours.1 The report underlines the role of families in promoting healthy habits in its guiding Consensus Statement, which was developed through a national multidisciplinary expert panel:
Families can support children and youth in achieving healthy physical activity, sedentary and sleep behaviours by encouraging, facilitating, modelling, setting expectations and engaging in healthy movement behaviours with them. Other sources of influence are important (e.g., child care, school, health care, community, governments) and can support families in these pursuits.2
As the report states, youth’s physical activity levels, is greatly influenced by family social support – particularly during early childhood. This support is shown to be most effective when taking self-regulatory approaches and when grounded in specific actions, such as setting goals together. Studies assert that parents who make clearly defined plans – how, when, where – to encourage their child’s healthy movement behaviours are more likely to follow through. As role models, parents can have a significant impact: every additional 20 minutes of physical activity by a parent can mean an additional 5 minutes in their child’s daily physical activity.3
Outdoor play and location linked to well-being
A growing body of research demonstrates the link between well-being and access to parks and green spaces. In 2017, the majority of households in Canada (87%) reported having a park within 10 minutes of their home. Of these households, almost all (85%) reported that they had visited the park within the previous 12 months. Among households that reported that they did not have nearby access (13%), 39% nevertheless reported visiting a park or green space in the previous 12 months.4
Research has shown that a neighbourhood’s built environment can have an impact on the time children spend outdoors, with lower traffic volumes, access to a yard and neighbourhood greenness all associated with more time spent by children playing outdoors in one study.5
Research from Statistics Canada has found a strong association between time spent outdoors and levels of physical activity among children, as well as a positive impact on psychosocial health and lower likelihood of experiencing peer relationship problems.6 More than one-third (36%) of surveyed parents with children aged 5–17 said that they play active games with their kids.7 Since the start of the pandemic, nearly two-thirds (62%) of youth in Canada cited exercising outdoors.8
Outdoor play can foster “freedom, fun, creativity, and skill- and confidence-building.”9 Whether it’s walking through a park, playing a game in the front yard or going for a jog, getting outdoors and practising healthy behaviours with family can play an important role in supporting physical activity and wellness at any time, but are particularly important as families continue to navigate the COVID‑19 pandemic and new and/or adapted ways of coming together.
Gaby Novoa is responsible for Communications at the Vanier Institute of the Family.
Nathan Battams is Communications Manager at the Vanier Institute of the Family.
Notes
- ParticipACTION, Family Influence: The 2020 ParticipACTION Report Card on Physical Activity for Children and Youth (June 17, 2020). Link: https://bit.ly/2Zser6r.
- Ibid.
- Ibid.
- Gordon Dewis, “Access and Use of Parks and Green Spaces: The Potential Impact of COVID‑19 on Canadian Households,” COVID‑19: A Data Perspective (June 9, 2020). Link: https://bit.ly/2CfuT0f.
- Amalie Lambert et al., “What Is the Relationship Between the Neighbourhood Built Environment and Time Spent in Outdoor Play? A Systematic Review,” International Journal of Environmental Research and Public Health (October 11, 2019). Link: https://bit.ly/2N8nan1.
- Richard Larouche et al., “Outdoor Time, Physical Activity, Sedentary Time, and Health Indicators at Ages 7 to 14: 2012/2013 Canadian Health Measures Survey,” Health Reports, Statistics Canada catalogue no. 82-003-X (September 21, 2016). Link: https://bit.ly/2N8VvlU.
- ParticipACTION, The Brain + Body Equation: Canadian Kids Need Active Bodies to Build Their Best Brains. The 2018 ParticipACTION Report Card on Physical Activity for Children and Youth (2018). Link: https://bit.ly/2Y7qjJR.
- Rubab Arim, Leanne Findlay and Dafna Kohen, “The Health and Behavioural Impacts of COVID‑19 on Youth: Results from the Canadian Perspectives Survey Series 1,” COVID‑19: A Data Perspective (May 15, 2020). Link: https://bit.ly/3e9rmyG.
- Lambert et al.
Food Insecurity and Family Finances During the Pandemic
Nadine Badets
June 12, 2020
The COVID‑19 lockdown and ensuing economic repercussions have created a significant amount of financial stress for families in Canada. Between February and April 2020, about 1.3 million people in Canada were unemployed, with approximately 97% of the newly unemployed on temporary layoff, meaning they expect to go back to their jobs once the pandemic restrictions are relaxed.1
Research has shown that financial insecurity can severely limit access to food for low income families and exacerbate socio-economic inequities.2 Other factors, such as health and disability status, level of social support and the limited availability of certain food products, also contribute to food insecurity during the COVID‑19 pandemic.
Financial inequities intensified during physical distancing and economic lockdown
Overall, 5.5 million adults in Canada have either been affected by job loss or reduced work hours during the COVID-19 lockdown, meaning these people and their households have a significant reduction in income for necessities such as food and shelter.3 In 2018, about 3.2 million people lived below Canada’s official poverty line,4 and the economic impacts of the pandemic have likely increased these numbers.
The pandemic is also amplifying existing financial inequities.5 In Canada in 2015, the national prevalence of low income was 14%, however it was much higher among some groups, such as immigrants (Arab, West Asian, Korean, Chinese), Indigenous Peoples (First Nations people, Inuit, Métis), and Black people.6, 7 These groups were more likely to be living with low income before the COVID‑19 lockdown, and have been more likely than others to report that the pandemic has had a negative effect on their finances. According to recent survey data from the Vanier Institute of the Family, the Association of Canadian Studies and Leger,8 over half of visible minorities (51%) had a decrease in their income during the lockdown, and Indigenous peoples (42%) were most likely to report having difficulty meeting financial obligations, such as being able to pay bills on time.9, 10
Food banks across Canada have seen surges in use since the beginning of the COVID‑19 pandemic
Prior to the COVID‑19 pandemic, Food Banks Canada estimated that food bank use across the country had stabilized, with 2019 having almost the same number of visits as 2018, remaining at levels similar to 2010. In the month of March 2019, there were close to 1.1 million visits to food banks across Canada, with more than 374,000 visits for feeding children.11
Statistics Canada estimates that in 2017–2018 about 9% of households (1.2 million) in Canada were food insecure, meaning they struggled financially to get food and did not have enough for all household members to eat regular and nutritious meals.12, 13 As with financial insecurity, food insecurity disproportionately affects certain population groups in Canada. For example, in 2014 food insecurity among Black people (29%) and Indigenous people (26%) was more than double the national average (12%).14
Research has consistently found that people living in remote and Northern communities are more likely to experience food insecurity, such as Inuit communities in Inuit Nunangat, the Inuit homeland.15 It has also been found that Indigenous populations living in urban areas experience high levels of food insecurity. In 2017, 38% of Indigenous peoples 18 years and older living in urban areas were food insecure.16
Since the COVID‑19 pandemic started, Food Banks Canada reported that there has been an average increase of 20% in demand for services from food banks across the country, alarmingly close to the 28% increase seen during the Great Recession. Projections by Food Banks Canada estimate that demand could continue to rise to between 30% and 40% higher than pre-pandemic levels. Some food banks – such as The Daily Bread in Toronto, one of the largest food banks in Canada – have seen increases of over 50% in use.17
Increases in grocery sales associated with the receipt of financial support through CERB
Early in the pandemic (late March to early April 2020), 63% of people reported that they stocked up on essential groceries and pharmacy products as a precaution.18
Grocery sales across Canada saw a sharp increase in March 2020, rising 40% toward the end of the month and continued to remain high in mid‑April.19 The delivery of federal financial supports for unemployed people, such as the Canadian Emergency Response Benefit (CERB),20 appear to be directly linked with an increase in grocery sales, which is likely helping to mitigate food insecurity for some Canadians.21
However, CERB currently only allows recipients to claim the benefit four times for a total of 16 weeks. As July 2020 approaches, many Canadians will be using up their final installment of CERB, and not all will be eligible to be transferred to EI, which could have a serious impact on food insecurity in Canada.
Single parents and seniors with low levels of social support struggle the most to get groceries
Physical (social) distancing measures have also created new barriers for individuals and families trying to navigate new rules of when, how and with whom they can or should buy groceries. For some, such as seniors, single parents, people with disabilities and those who have (or are caring for someone with) compromised immune systems, having limited finances and little social support can seriously restrict access to food.
In 2017–2018, single parents with children under 18 years reported the highest levels of food insecurity in Canada. Female single parents had the highest rate of food insecurity at 25%, followed by male single parents at 16%.22 This compares with 12% among men and women living alone, 7% of couples with children under 18, and 3% of couples without children.23
Physical distancing measures can be particularly complex for single parents without access to child care, who may have to decide between bringing children to grocery stores, thereby breaking physical distancing rules and potentially exposing children to the virus, or turning to organizations like food banks for support.24
Seniors living with low income are less likely to have a high level of social support (77%) compared with seniors living in high income (89%). In periods of isolation such as the current lockdown, access to essentials like food can be challenging, especially for low income seniors who are ill, concerned for their health or unable to get groceries on their own due to physical or financial restrictions.25
Hoarding of certain foods limits supply and access for low income families and food banks
The COVID‑19 pandemic brought a series of panic-buying trends around the world, most notably of hand sanitizer and toilet paper.26 Many grocery stores and pharmacies have had their stock of certain food items depleted several times during the pandemic.
In mid-March 2020, sales of dry and canned foods in Canada surpassed those of fresh and frozen foods. Rice sales rose 239% compared with the same period in 2019, sales of pasta rose by 205%, canned vegetables by 180% and sales of infant formula by 103%.27 Shelf-stable foods such as these are usually a major part of food bank products,28 but are more difficult to come by during the pandemic and thus limit supplies for food insecure families.29
More research is needed to better understand the effects of the pandemic on hunger, nutrition and food insecurity in households across Canada in order to support and develop programs aimed at reducing inequities in access to food.
To find a food bank nearby or make a donation, visit the Food Banks Canada website.
Nadine Badets, Vanier Institute on secondment from Statistics Canada
Notes
- Statistics Canada, “COVID‑19 and the Labour Market in April 2020,” Infographics (May 8, 2020). Link: https://bit.ly/3duO2si.
- Visit the PROOF Food Insecurity Policy Research website for more on food insecurity and social inequities. Link: https://bit.ly/2MQH8T8.
- Statistics Canada, “COVID‑19 and the Labour Market in April 2020.”
- Statistics Canada, “Health and Social Challenges Associated with the COVID‑19 Situation in Canada,” The Daily (April 6, 2020). Link: https://bit.ly/3fErrvo.
- Learn about the impact of the COVID-19 pandemic on inequalities in Canada, see Canadian Human Rights Commission, Statement – Inequality Amplified by COVID-19 Crisis (March 31, 2020).
- Statistics Canada, “Visible Minority (15), Income Statistics (17), Generation Status (4), Age (10) and Sex (3) for the Population Aged 15 Years and Over in Private Households of Canada, Provinces and Territories, Census Metropolitan Areas and Census Agglomerations, 2016 Census – 25% Sample Data,” Data Tables, 2016 Census (updated June 17, 2019). Link: https://bit.ly/30OqUC2.
- Statistics Canada, “Aboriginal Identity (9), Income Statistics (17), Registered or Treaty Indian Status (3), Age (9) and Sex (3) for the Population Aged 15 Years and Over in Private Households of Canada, Provinces and Territories, Census Metropolitan Areas and Census Agglomerations, 2016 Census – 25% Sample Data,” Data Tables, 2016 Census (updated June 17, 2019). Link: https://bit.ly/2zPHMxb.
- The survey, conducted by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, on March 10–13, March 27–29, April 3–5, April 10–12, April 17–19, April 24–26, May 1–3 and May 8–10, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. All samples, with the exception of those from March 10–13 and April 24–26, also included booster samples of approximately 500 immigrants. In addition, from about May 1 to 10, there was an oversample of 450 Indigenous peoples. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- It is important to emphasize that there is a great deal of diversity within visible minority groups and Indigenous populations, all groups have unique and distinct experiences of financial and food insecurity, as well as histories, geographies, cultures, traditions, and languages.
- For more on the impact of the COVID-10 pandemic on immigrant families and First Nations people, Métis and Inuit, see Laetitia Martin, Families New to Canada and Financial Well-being During Pandemic (May 21, 2020) and Statistics Canada, “First Nations people, Métis and Inuit and COVID-19: Health and social characteristics,” The Daily (April 17, 2020). Link: https://bit.ly/2Y714r3.
- Food Banks Canada, “Hunger Count 2019.” Link: https://bit.ly/2AZ1GpP.
- Ibid.
- Statistics Canada, “Household Food Security by Living Arrangement,” Table 13-10-0385-01 (accessed May 27, 2020). Link: https://bit.ly/37iQDnq.
- Health Canada, Household Food Insecurity in Canada: Overview (page last updated February 18, 2020). Link: https://bit.ly/30JLCDh.
- Valerie Tarasuk, Andy Mitchell and Naomi Dachner, “Household Food Insecurity in Canada, 2014,” PROOF Food Insecurity Policy Research (updated May 12, 2017). Link: https://bit.ly/3eJ0mpl (PDF).
- Paula Arriagada, “Food Insecurity Among Inuit Living in Inuit Nunangat,” Insights on Canadian Society, Statistics Canada catalogue no. 75-006-X (February 1, 2017). Link: https://bit.ly/2maW9oN.
- Paula Arriagada, Tara Hahmann and Vivian O’Donnell, “Indigenous People in Urban Areas: Vulnerabilities to the Socioeconomic Impacts of COVID‑19,” STATCAN COVID‑19: Data to Insights for a Better Canada (May 26, 2020). Link: https://bit.ly/2zuTgWT.
- Beatrice Britneff, “Food Banks’ Demand Surges Amid COVID‑19. Now They Worry About Long-Term Pressures,” Global News (April 15, 2020). Link: https://bit.ly/3boEHRe.
- Statistics Canada, “How Are Canadians Coping with the COVID‑19 Situation?,” Infographic (April 8, 2020). Link: https://bit.ly/2WKdx21.
- Statistics Canada, “Study: Canadian Consumers Adapt to COVID‑19: A Look at Canadian Grocery Sales Up to April 11,” The Daily (May 11, 2020). Link: https://bit.ly/3cj58Jz.
- In April 2020, Canada’s federal government established the Canada Emergency Response Benefit (CERB), which provides $2,000 every four weeks to workers who have lost their income as a result of the pandemic. This benefit covers those who have lost their job, are sick, quarantined, or taking care of someone who is sick with COVID‑19. It applies to wage earners, contract workers and self-employed individuals who are unable to work. The benefit also allows individuals to earn up to $1,000 per month while collecting CERB. As a result of school and child care closures across Canada, the CERB is available to working parents who must stay home without pay to care for their children until schools and child care can safely reopen and welcome back children of all ages. Government of Canada, “Canada’s COVID-19 Economic Response Plan.” Link: https://bit.ly/2AhY1DD.
- Statistics Canada, “Study: Canadian Consumers Adapt to COVID‑19: A Look at Canadian Grocery Sales Up to April 11.”
- Statistics Canada, “Household Food Security by Living Arrangement.”
- Ibid.
- Ottawa Food Bank, “COVID‑19 Response Webinar – The First 5 Weeks” (May 13, 2020). Link: https://bit.ly/2AWXF55.
- Kristyn Frank, “COVID‑19 and Social Support for Seniors: Do Seniors Have People They Can Depend on During Difficult Times?,” StatCan COVID‑19: Data to Insights for a Better Canada (April 30, 2020). Link: https://bit.ly/3biLMmp.
- Statistics Canada, “Canadian Consumers Prepare for COVID‑19,” Price Analytical Series (April 8, 2020). Link: https://bit.ly/2WO1r86.
- Ibid.
- Food Banks Canada, “Support Your Local Food Bank.” Link: https://bit.ly/3gqmYwG.
Families in Canada Adapting: A Wedding at a Distance
While the COVID-19 pandemic has affected families across Canada and the social, economic, cultural and environmental contexts that impact their well-being, it hasn’t stopped family life by any means.
Whether it’s managing work–family responsibilities, connecting to celebrate milestones or providing support in difficult times, people are finding diverse and creative ways to keep doing what families do.
As families in Canada continue to manage these transitions, the Vanier Institute of the Family is gathering, compiling and sharing these “stories behind the statistics” to provide insights and into family strengths, resilience and diverse experiences across the country.
A Wedding at a Distance
Edward Ng, PhD
June 1, 2020
In early May, I had my first experience attending an online wedding. The event was planned long ago, well before the COVID‑19 pandemic had been declared. Once the restriction order was imposed in mid-March, the couple adjusted the wedding plan so that the event could be held online instead.
The ceremony, which was held in Montreal at the home of the bride, was ultimately broadcast through YouTube all over the world. Will this be the trend of the future? Before this, my only “virtual family gathering” was a funeral for my uncle who passed away a few years ago in Sydney, Australia.
The ceremony started at 10:30 a.m. on a Saturday morning (or wherever it happened to be for the online guests). After introductory music, the flower girl and the ring bearer made their entry into the broadcasting not by walking down the aisle in a church but rather their own corridor at home, throwing flowers and small decorations along the way. Then followed the well-arranged performance by a quartet, assembled online playing musical pieces for the occasion. The quartet was followed by a choir singing separately yet harmoniously, from wherever they were. Then came the sharing from ministers, followed by exchanging of vows and of rings and the signing of the marriage certificate. The ceremony took just more than an hour, and concluded with selfie-taking (so to speak).
In the joy of the moment, though, neither the family nor the guests – nor the bride and groom – cared whether we were there virtually. Not everything was the same – when it came to attire, some of us still chose to dress up for the occasion with formal dress or suit jacket, while others chose to dress casually. People were adapting as they saw fit as we all experienced this together, while apart.
The YouTube broadcasting feature was used, which allowed for viewers all over the world to contribute to the occasion in live time. From the beginning of the online ceremony, we observed many congratulatory wishes and comments beaming through. Family, friends and loved ones from Montreal, Ottawa and Toronto, as well as the United States, Europe, Australia and Asia, left their wishes to the couple. One guest commented that this was the first time that people at a wedding were able to contribute their comments and appreciation of the occasion so instantaneously.
By bringing the wedding online, more people were able to attend, some of whom wouldn’t have been able to come otherwise. For my own family, Montreal is at least a two- to three-hour drive each way; for those observing from Asia, however, that would be at least two days of travel to and from (with much higher fares, if flying has been allowed). Furthermore, these international travellers would have had to quarantine for at least 14 days. That would have made attending this wedding from overseas quite impossible.
At the end of the event, the newlyweds expressed their appreciation to the online wedding planning team, and promised that there will be wedding celebration activities after the restriction order has been lifted. We all looked forward to this day, and ultimately had a positive experience with this online family event. In this case, moving the wedding ceremony online was necessary, practical and sensible, especially in view of pandemic. Time will tell whether online family milestones will be a norm in the future.
Edward Ng, PhD, Vanier Institute on secondment from Statistics Canada
Family Finances and Mental Health During the COVID‑19 Pandemic
Ana Fostik, PhD, and Jennifer Kaddatz
May 26, 2020
In March 2020, the coronavirus pandemic suddenly brought social and economic activities to a halt across Canada, with data showing serious impacts on labour market activity. Recent estimates from Statistics Canada show that 1 million fewer Canadians were employed in March than in February, and the usual labour market activity of 3.1 million Canadians was affected (i.e. worked fewer hours or lost their job).1
According to survey data for April 10–12, 2020 from the Vanier Institute of the Family, the Association for Canadian Studies (ACS) and Leger,2 38% of men and 34% of women aged 18 and older said that they lost their job temporarily or permanently, or experienced pay or income losses, due to the COVID-19 pandemic. Consequently, 27% of men and 25% of women reported a negative financial impact (i.e. ability to pay mortgage or rent and/or their bills).
Not surprisingly, Statistics Canada recently found that adults who suffered a major or moderate impact of the pandemic were much more likely to report fair or poor mental health than those who were less impacted (25% and 13%, respectively).3
Data collected in mid-April by the Vanier Institute of the Family, the Association for Canadian Studies and Leger show that younger adults have been particularly affected: more than half (52%) of those aged 18–34 reported a negative impact on their labour market activity (job or pay/income losses), compared with 39% of those aged 35–54 and 21% of those aged 55 and older. This is reflected in the shares of adults experiencing immediate negative financial outcomes, which were reported by 33% of adults under 55 and 15% of those over 55.
Adults in financial difficulty are more likely to report mental health issues
Among the core working age population (aged 18–54), just over half reported feeling anxious or nervous (53%), irritable (49%) or sad (48%) often or very often during the COVID-19 pandemic, according to the Vanier Institute/ACS/Leger survey. Four in 10 reported difficulty sleeping (40%) and having mood swings (40%) often or very often.
Among those who experienced immediate negative outcomes, such as not being able to pay rent or mortgage and/or their bills, about 6 in 10 reported anxiety or nervousness (63%), irritability (60%) or sadness (57%) often or very often, whereas half said they have had difficulty sleeping (50%) or experience mood swings (52%) often or very often (fig. 1).
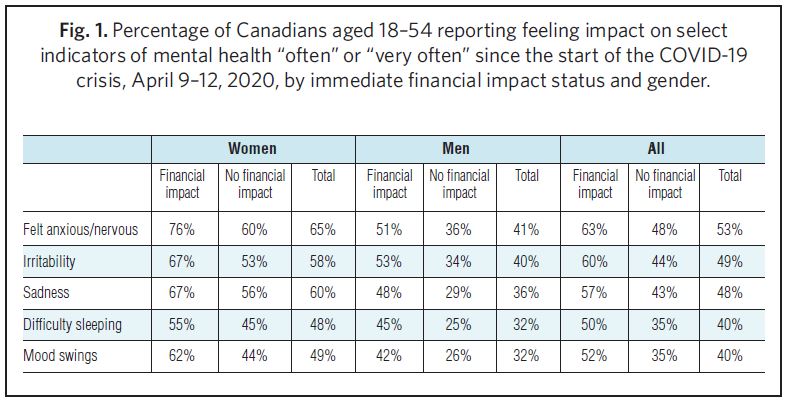
Women in financial difficulty suffer from mental health issues in higher shares than men
According to the 2018 Canadian Community Health Survey, women were slightly less likely than men to report excellent/good mental health (66% and 71%, respectively).4 During the coronavirus pandemic, however, Statistics Canada found a much larger difference, at 49% of women and 60% of men.5
Vanier Institute/ACS/Leger survey data show women aged 18–54 reporting specific mental health issues often or very often in much larger shares than men of the same age. About 6 in 10 women reported experiencing anxiety or nervousness, irritability or sadness often or very often, compared with 4 in 10 men. Similarly, about half women experienced difficulty sleeping or mood swings often or very often, compared with 3 in 10 men (fig. 1).
This difference by gender in reporting mental health issues is maintained even when examining the proportions of men and women who suffered immediate negative financial outcomes and those who did not. For instance, three-quarters of women (76%), compared with half of men (51%), who had difficulty paying mortgage or rent and/or their bills reported feeling nervous or anxious often or very often. Almost 7 in 10 women in financial difficulty experience irritability (67%) or sadness (67%), compared with about half of men in the same situation (53% and 48%, respectively) (fig. 1).
About 6 in 10 of women in financial difficulty (55% and 62%) suffered difficulty sleeping and had mood swings often or very often, compared with 4 in 10 men in the same situation (45% and 42%, respectively) (fig. 1).
Adults with financial difficulties report similar mental health issues, whether living with young children or not
If women are significantly less likely than men to report positive mental health during the pandemic, even when financial outcomes are controlled for, what factors might be at play in creating these gender differences? Could these mental health challenges be related to family responsibilities?
An analysis of the April 10–12, 2020 data indicates that heightened symptoms of poor mental health do not appear to be linked to the presence of children in the home. Women who live with children aged 12 and younger in the household report experiencing anxiety (69%), irritability (60%), sadness (59%), difficulty sleeping (51%) and mood swings (51%) often and very often in similar proportions as women who do not live with children (63%, 57%, 60%, 47% and 48%, respectively). Men who live with young children also report these problems in similar proportions as those who do not (fig. 2).

Among women in financial difficulty, there is little difference in the share reporting any of these mental health problems whether they have young children living in the household or not. This is also true among women who did not experience immediate negative financial outcomes: living with children aged 12 and under in the household does not appear to make a difference (fig. 2).
Analysis of self-reported mental health status shows that some of the differences by gender persist when controlling for province of residence, age, financial difficulty, job/pay loss, presence of children aged 12 and under, household income, marital status and educational attainment. Controlling by these variables and compared with men who are in financial difficulty, women in financial difficulty are about twice as likely to suffer from anxiety, sadness or mood swings. Among adults who have not suffered financial negative outcomes, there are no significant differences between men and women in mental health outcomes once controlling for these factors.
While this analysis could not pinpoint potential reasons why women are more likely than men to report poor mental health symptoms, future research may seek to focus on psychological differences between women and men in crisis situations in order to determine whether or not women and men react differently in crisis situations or when there is an immediate threat to personal or family health and well-being. More research on the impact of gendered aspects of household work and caregiving, including the mental burden associated with these types of unpaid work, might also shed light on these differences.
Ana Fostik, PhD, Vanier Institute on secondment from Statistics Canada
Jennifer Kaddatz, Vanier Institute on secondment from Statistics Canada
Notes
- Statistics Canada, “The Impact of COVID-19 on the Canadian Labour Market,” Infographics (April 9, 2020). Link: https://bit.ly/3geJKro.
- A survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, conducted March 10–13, March 27–29, April 3–5, April 10–12, April 17–19 and April 24–26, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. All samples, except for the March 10–13 and April 24–26 samples, also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Statistics Canada, “Canadian Perspectives Survey Series 1: Impacts of COVID-19 on Job Security and Personal Finances, 2020,” The Daily (April 20, 2020). Link: https://bit.ly/2Y9y42h.
- Leanne Findlay and Rubab Arim, “Canadians Report Lower Self-Perceived Mental Health During the COVID-19 Pandemic,” STATCAN COVID-19: Data to Insights for a Better Canada, Statistics Canada catalogue no. 45280001 (April 24, 2020). Link: https://bit.ly/2xMorvZ.
- Ibid.
Parents’ Thoughts on Post-Pandemic Future in Canada
Nadine Badets
May 6, 2020
The COVID-19 pandemic restrictions have transformed family life in Canada. With the closure of schools, daycares, restaurants and many businesses, as well as major job losses and new work-from-home measures, many parents and children are spending a lot more time together.
So how do families feel about life after the pandemic? Six weeks of data from the Vanier Institute of the Family, the Association for Canadian Studies and Leger show that families with children are not ready to send them back to school this year, but parents are ready to go back to their workplaces after the pandemic, among other findings from this ongoing series of surveys.1
Fear of coronavirus greater among families caring for children
As of May 6, 2020, children and youth 19 years and younger represent a small portion of COVID-19 cases in Canada (5%).2 Nevertheless, almost 30% of adults living with children and youth under 18 are very afraid that someone in their immediate family will contract COVID-19, compared with 22% of people not living with children3 (fig. 1).

Even so, more than half of adults living with children (56%) said they would support a government policy that relaxes social (physical) distancing restrictions for everyone under 65, whereas 42% of people living without children said they would support this policy.
Most parents don’t want children to attend summer school to catch up
Over 80% of parents are living with their children during the pandemic, and 7% are sharing custody of their children with a parent in a separate household. Six in 10 parents (60%) reported they are now talking to their children more often than before the lockdown. Parents of school-aged children are also navigating the education system with their children as newly instated teachers, tutors and homework helpers. Home schooling is challenging for many families,4 raising concerns about students falling behind.
Most provinces have not yet announced plans to reopen schools, whereas all three territories have confirmed they will keep schools closed until September. However, Quebec has pledged to reopen most elementary schools on May 11 and, as of April 29, 2020, Ontario and Nova Scotia have tentative opening dates closer to June, but their deadlines keep shifting.5 When surveyed, two-thirds (66%) of parents indicate that even if schools in Canada open before the end of June, they would prefer for their children to return to school in September, rather than attend school over the summer (July and/or August) to catch up for missed time.
More than half of parents are ready to return to work but don’t want to use public transit
The COVID-19 pandemic has created enormous job losses across the country,6 and parents living with children who view the COVID-19 outbreak as a “major threat” to their jobs were more likely to report feeling sad and anxious or nervous, compared with people living without children.7
Of those still employed, people living with children were more likely to report satisfaction with the measures their employer put in place to fight COVID-19 (59%) than people without children (37%). This could be because they can work from home and care for their children given that daycares and schools are closed. About 55% of adults living with children reported they are now working from home (fig. 2). People living with children were also more likely to say they would be comfortable returning to their workplace once the COVID-19 restrictions are lifted (54%) than people without children (37%).
However, more than 60% of parents said they would not be comfortable riding public transit, even when COVID-19 restrictions start being relaxed, which could have implications for commuting once people return to their workplace (fig. 3). Adults living with children were more likely to say they would prefer to commute to work only when needed (39%) than people without children (27%).
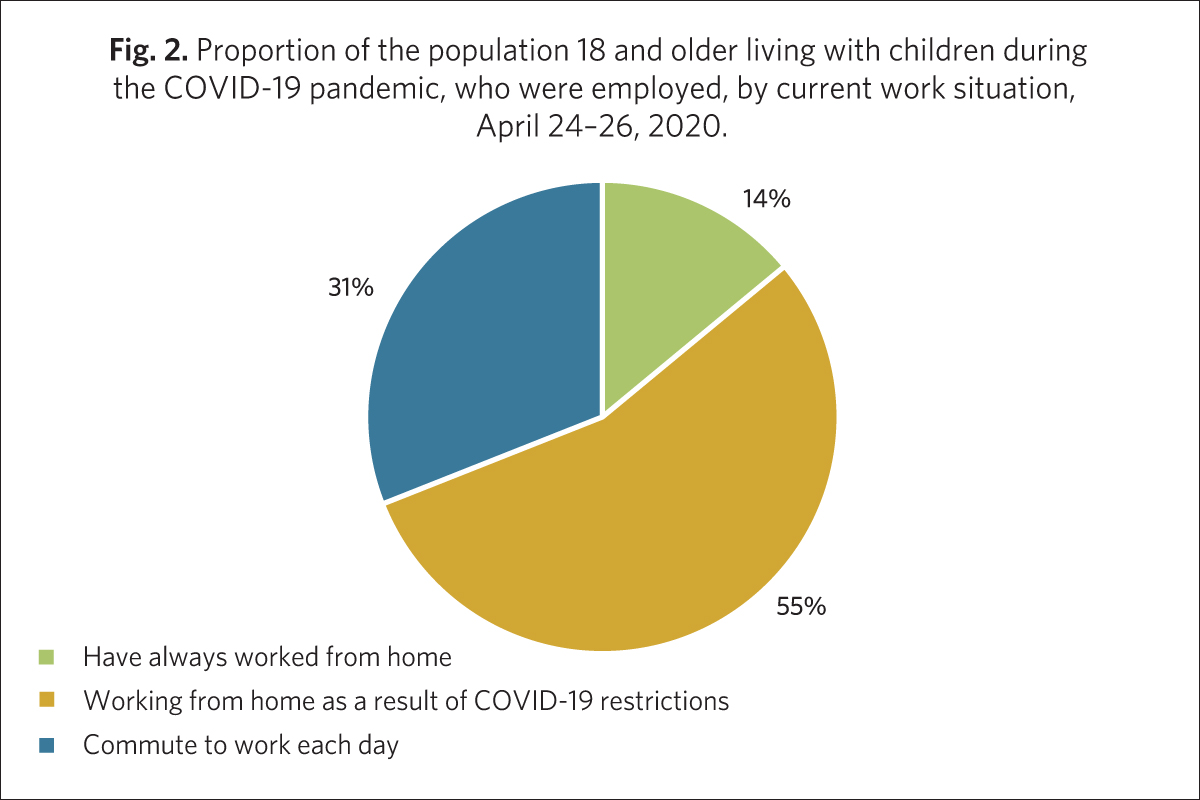
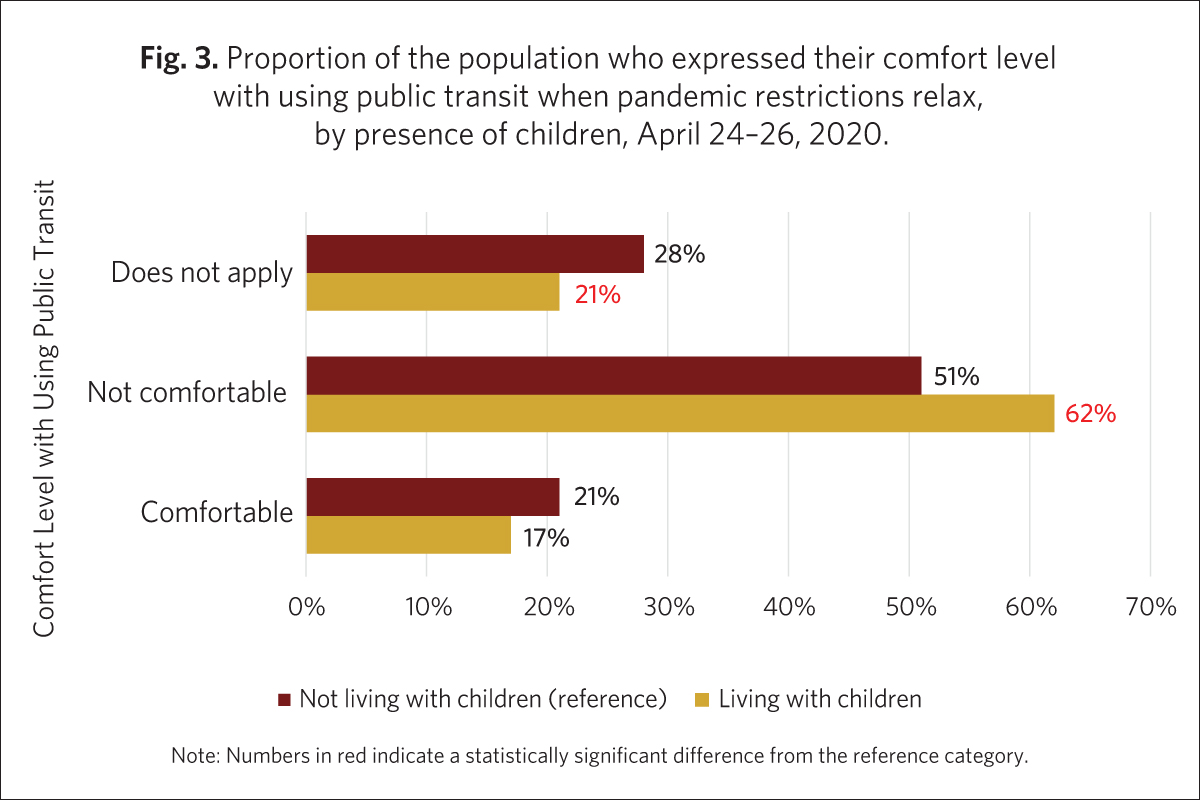
Parents abandoning vacation plans, most won’t travel in 2020
In addition to expressing discomfort with commuting in public transit, parents are also not comfortable with travel. About 6 in 10 (59%) adults living with children reported that they had to change vacation plans due to the 2020 coronavirus pandemic, which was likely affected by Canada’s lockdown and borders closing around March break. When asked if they now plan to take a vacation during 2020, 72% of parents said it was unlikely.
Nadine Badets, Vanier Institute on secondment from Statistics Canada
Notes
- A survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, conducted March 10–13, March 27–29, April 3–5, April 10–12, April 17–19 and April 24–26, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. All samples except for the March 10–13 and April 24–26 samples also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Public Health Agency of Canada, Coronavirus Disease 2019 (COVID-19): Epidemiology Update (accessed May 6, 2020). Link: https://bit.ly/2yXbD68.
- See note 1.
- Jessica Wong, “Frustrated Parents in Ontario Pivot from Official Distance-Learning Program Amid COVID-19,” CBC News (April 30, 2020). Link: https://bit.ly/3aTOMFR.
- CBC Kids News, When Will Your School Reopen? Check Out This Map (April 29, 2020). Link: https://bit.ly/2KMhcGW.
- Statistics Canada, “Labour Force Survey, March 2020,” The Daily (April 9, 2020). Link: https://bit.ly/2YABzPR.
- Jennifer Kaddatz, “Families Struggle to Cope with Financial Impacts of the COVID-19 Pandemic,” Vanier Institute of the Family (April 9, 2020).
Families in Canada Express “Major Concern” for Senior Health and Well-being During COVID-19
Nadine Badets and Ana Fostik, PhD
April 30, 2020
The Public Health Agency of Canada identifies older adults as being particularly vulnerable to COVID-19 and at high risk for severe illness and death.1 In 2019, 9.1 million people in Canada were aged 60 and older, representing about one-quarter of the total population.2
As of April 27, 2020, about 37% of confirmed COVID-19 cases in Canada were diagnosed in adults aged 60 and older, and this age group accounted for more than half (56%) of all coronavirus cases with pneumonia. Adults aged 60 and older had the highest proportions of severe outcomes with 66% of reported COVID-19 hospitalizations, 63% of Intensive Care Unit (ICU) admissions and 95% of deaths.3
The higher susceptibility of older adults to the virus has created heightened levels of stress for seniors and their families and caregivers as they navigate the COVID-19 pandemic.
Key facts and statistics
- Approximately 37% of confirmed COVID-19 cases in Canada were diagnosed in adults aged 60 and over (April 27, 2020).
- Adults aged 60 and over have accounted for 66% of reported COVID-19 hospitalizations, 63% of Intensive Care Unit (ICU) admissions and 95% of deaths (April 27, 2020).
- 70% of adults aged 18 and older indicated that they are somewhat/very afraid that a member of their immediate family will contract COVID-19 (April 27, 2020).
- 15% indicated that some senior relatives are currently living in nursing homes or long-term care facilities, 85% of whom expressed concern about the health of these family members (April 27, 2020).
- Nearly 8 in 10 (79%) of coronavirus deaths in Canada occurred in nursing and long-term care homes (April 28, 2020).
Families with senior relatives in nursing homes are most concerned
In a survey conducted on April 17–19, 2020 by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, close to 70% of adults aged 18 and older indicated that they are somewhat or very afraid that a member of their immediate family will contract COVID-19.4 For context, in 2018 Statistics Canada found that about 7.8 million adults aged 15 and older provided care to a family member or friend,5 and almost 4 in 10 care recipients in Canada 2018 were aged 65 and older.6
During the COVID-19 pandemic, 11% of adults reported that at least one senior relative was living with them.7 Close to 47% indicated that the seniors in their family live in their own separate homes, and 15% indicated that some senior relatives are currently living in nursing homes or long-term care facilities.
Most adults (85%) whose senior family members live in care facilities expressed concern about the health of these family members, while a slightly lower share of adults who live with seniors (77%), or whose senior family members live in separate homes (72%), expressed concerned for their health.
Seniors in long-term care facilities are struggling to cope with pandemic restrictions
A large part of the devastation caused by the coronavirus pandemic has been occurring in nursing homes and long-term care facilities. Dr. Theresa Tam, Canada’s Chief Public Health Officer, announced in mid-April 2020 that about half of COVID-19 deaths in Canada have been linked to outbreaks in long-term care homes for seniors,8 and, as of April 28, 2020, nearly 8 in 10 (79%) of coronavirus deaths in Canada occurred in nursing and long-term care homes.9
Almost 61% of relatives reported that they are somewhat or very worried about the quality of care seniors are receiving in nursing homes and long-term care facilities. Furthermore, close to two-thirds (63%) of adults whose senior relatives live in long-term care homes think these family members are having a somewhat or very difficult time coping with COVID-19 restrictions, such as staying in their rooms and no contact/visits from others. About 12% aren’t sure how their relatives are coping with the restrictions.
Nadine Badets, Vanier Institute on secondment from Statistics Canada
Ana Fostik, PhD, Vanier Institute on secondment from Statistics Canada
Notes
- Public Health Agency of Canada, People Who Are at High Risk for Severe Illness from COVID-19 (April 20, 2020). Link: https://bit.ly/2SjxfAz.
- Statistics Canada. Population Estimates on July 1, by Age and Sex (Table 17-10-0005-01). Link: https://bit.ly/2VA2TeX.
- Public Health Agency of Canada, Coronavirus Disease 2019 (COVID-19): Epidemiology Update (April 29, 2020). Link: https://bit.ly/3cPclRD.
- A survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, conducted March 10–13, March 27–29, April 3–5, April 10–12 and April 17–19, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. All samples except for the March 10–13 sample also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Statistics Canada, “Caregivers in Canada, 2018,” The Daily (January 8, 2020). Link: https://bit.ly/2NKyQgc.
- Statistics Canada, “Care Counts: Care Receivers in Canada, 2018,” Infographics, Statistics Canada catalogue no. 11-627-M (January 22, 2020). Link: https://bit.ly/2TNql8c.
- April 17–19 survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger (see note 4).
- Olivia Bowden, “Long-Term Care Homes with the Most Coronavirus Deaths in Canada,” Global News (April 17, 2020). Link: https://bit.ly/2Y2Lihn.
- Beatrice Britneff and Amanda Connolly, “Coronavirus Spread Slowing in Canada; Death Rate Rises Due to Long-Term Care Fatalities,” Global News (April 28, 2020). Link: https://bit.ly/2xlWjQ4.
Health Habits During the COVID-19 Pandemic
Jennifer Kaddatz and Nadine Badets
April 27, 2020
Canada’s lockdown for the COVID-19 pandemic has placed heavy restrictions on individuals and businesses, which have altered many commonplace activities, from preparing and consuming foods to shopping, exercising and spending time outdoors. The health of adults in Canada is changing, and not just because of the virus, but also because of pre-existing and newly emerging health habits.
Throughout this period of social isolation, adults are spending more time preparing meals and drinking alcohol at home, but spending less time exercising and going outside, according to four weeks of recent survey data from the Vanier Institute of the Family, the Association for Canadian Studies and Leger1 and other pandemic data sources.
These patterns will be important to watch throughout the duration of the pandemic, given the potential impacts on both physical and mental health among families across the country.
About 4 in 10 adults spend more time preparing meals at home
Healthy eating is fundamental to good health, is a key element in healthy human development and is important in reducing the risk of many chronic diseases. Preparing and cooking food at home can reduce the amount of sodium, sugar and saturated fat in meals while at the same time increasing the intake of vegetables, fruit, whole grains and plant-based proteins. On the other hand, eating out or ordering in can negatively impact a person’s health because of the potential for the meals to be more highly processed, with lower quantities of vegetables, fruits and whole grain foods.2
Not surprisingly, during COVID-19 isolation more people in Canada are eating home-cooked meals. In fact, 41% of adults say that they are spending more time preparing meals now than they were before the pandemic, according to April 9–12 data (fig. 1). Women, in particular, seem to be spending more time in the kitchen, with 44% saying they are preparing meals “more often” as compared with 38% of men. In fact, nearly half (48%) of women aged 35–54 are spending more time preparing meals, as are 44% of men in that age group.

In contrast, a lower share of women (18%) than men (24%) picked up take-out food from a restaurant in the week before the April 9–12 survey, although women are about equally as likely (18% vs. 16%) to get food delivered to their home or business (figs. 2 and 3). Young men, aged 18–34, are most likely to pick up take-out food (24%) in the past week, whereas young women aged 18–34 are the gender/age group most likely to order in (27%).


One in 5 adults are drinking more alcohol at home
Alcohol can have significant consequences for physical and mental health if consumed in large quantities, by exacerbating pre-existing mental health issues, increasing the short-term risk of injury or acute illness, and increasing the long-term risk of serious diseases like liver disease and some cancers.3 Accordingly, if alcohol consumption goes up during the coronavirus crisis, there could be significant post-pandemic impacts on individual and family health and on the health care system in Canada.
A survey by Statistics Canada carried out March 29–April 3 found that 20% of Canadians aged 15–49 are drinking more at home during the COVID-19 pandemic than they were before it started.4 Similarly, a March 30–April 2 poll by Nanos/Canadian Centre on Substance Use and Addiction found that 21% of adults aged 18–34 and 25% of those aged 35–54 have started drinking more at home since the start of the COVID-19 crisis.5
Respondents to the Nanos poll who report staying home more and consuming more alcohol say that their drinking has increased most often because of the lack of a regular schedule (51%), boredom (49%), stress (44%) and/or loneliness (19%).
According to data collected April 9–12 by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, 14% of adults had gone to a liquor store in the previous week, with more men (18%) having done so than women (11%).
Nearly 4 in 10 are exercising less often
Although being confined to home may have increased the amount that adults are drinking, it does not seem to have increased the amount that they are exercising.
On the contrary, nearly 4 in 10 women (38%) and 33% of men say as of April 9–12 that they are exercising “less often” now than they were before pandemic. People living in Quebec (42%) most commonly report a decrease in their frequency of exercise as compared with those in the other provinces.
Notably, it appears that younger families may be spending more time exercising. A greater share of adults who live with children (23%) report they are exercising more often since the pandemic began compared with those who were not living with children (18%) (fig. 4). Additionally, nearly 3 in 10 adults aged 18–34 (28%) say that they were exercising more often since the start of the crisis compared with 14% of adults 55 years and older.

Increased COVID-19 anxiety and decreased exercise may be linked
According to the Canadian Psychological Association, regular physical activity can reduce day-to-day stress, can prevent depression and anxiety disorders, and may be as effective as psychological and pharmaceutical treatments for depression and anxiety.6 At the same time, however, mental health challenges, such as anxiety and depression, can also make it difficult to adopt or continue with an exercise program, particularly during unusual times.
In fact, April 9–12 data reveal that people who “very often” report anxiety or nervousness during the COVID-19 crisis are more likely to say they are exercising “less often” (20%) now than they were before the pandemic, whereas 13% say they are exercising “equally as often” as before the COVID-19 crisis started.
In comparison, adults who say that they have felt anxious or nervous “not often at all” since the beginning of the pandemic are more likely to say that the frequency with which they exercise has not changed since the start of the pandemic (24%) than to say that they are exercising more often (17%) or less often (17%) now.
Almost half of adults are going outside less often
Spending time outdoors in nature has a significant impact on mental health and wellness.7 Furthermore, in 2016, Statistics Canada’s General Social Survey found that 7 in 10 Canadians participated in one or more outdoor activities, showing that spending time outdoors is an important part of Canadian lifestyles.8
Nevertheless, during the COVID-19 pandemic, almost half of women (46%) and men (45%) say that they are going outside less often now than they were before the crisis. The shares of those saying they are going outside less often vary by province, from a low of 39% in Quebec and Manitoba/Saskatchewan to a high of 49% in Ontario.
What is of particular interest, however, is the variation in the share of people going outside less often by urban or rural area of residence. More than half (54%) of urban dwellers indicate that they are going outside less often now than before the pandemic, compared with 45% of suburban adults and 29% of people living in rural areas.
At the other end of the spectrum, when it came to those who say they are going outside more often, a higher proportion of women (25%) than men (15%) report a positive change.
It will be interesting to see, as spring changes to summer, whether the shares of people in Canada who are going outside, and who are exercising more often, increase with the warmer temperatures.
Jennifer Kaddatz, Vanier Institute on secondment from Statistics Canada
Nadine Badets, Vanier Institute on secondment from Statistics Canada
Notes
- The survey, conducted March 10–13, March 27–29, April 3–5 and April 9–12, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. The March 27–29, April 3–5 and April 9–12 samples also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Health Canada, Canada’s Food Guide. Link: https://bit.ly/2VsffFO.
- Peter Butt, Doug Beirness, Louis Gliksman, Catherine Paradis and Tim Stockwell, Alcohol and Health in Canada: A Summary of Evidence and Guidelines for Low Risk Drinking. Ottawa, ON: Canadian Centre on Substance Abuse (November 25, 2011). Link: https://bit.ly/3avfCne (PDF).
- Statistics Canada, “How Are Canadians Coping with the COVID-19 Situation?” Infographics (April 8, 2020). Link: https://bit.ly/2wVzkuL.
- Nanos conducted an RDD dual frame (land- and cell-lines) hybrid telephone and online random survey of 1,036 Canadians, 18 years of age or older, between March 30 to April 2, 2020 as part of an omnibus survey. Participants were randomly recruited by telephone using live agents and administered a survey online. The margin of error for this survey is ±3.1 percentage points, 19 times out of 20. The research was commissioned by the Canadian Centre on Substance Use and Addiction and was conducted by Nanos Research. Link: https://bit.ly/3aybEue (PDF).
- Canadian Psychological Association, “Psychology Works” Fact Sheet: Physical Activity, Mental Health, and Motivation (November 2016). Link: https://bit.ly/2yvVXXb (PDF).
- Canadian Parks Council, Connecting Canadians with Nature: An Investment in the Well-Being of Our Citizens (2014). Link: https://bit.ly/2SIeu9q.
- Statistics Canada, Canadians and the Outdoors (March 26, 2018). Link: https://bit.ly/34VPdy1.
Do Adults in Couples Have Better Mental Health During the COVID‑19 Pandemic?
Ana Fostik, PhD, and Jennifer Kaddatz
April 22, 2020
Nearly half of adults aged 18 years or older in Canada report feeling anxious/nervous (47%) or sad (45%) “very often” or “often” since the beginning of the COVID-19 crisis, according to survey data from the Vanier Institute of the Family, the Association for Canadian Studies and Leger, which was collected from April 9 to 12, 20201 (fig. 1).
Four in 10 report feeling irritable (39%) and about one-third report experiencing sleep-related problems (35%) and mood swings (32%) “very often” or “often” since the start of the crisis (fig. 1).
But are adults currently in a couple – whether common-law or married – as likely as those who are single or separated, divorced or widowed to experience feelings of unsettledness?
Anxiety/nervousness and difficulty sleeping during the pandemic don’t appear to be linked to marital status
Feeling anxious or nervous very often/often is equally likely to be reported by adults who are part of a couple (48%) as by those who are single (47%) or separated, divorced or widowed (43%) (fig. 1).
Similarly, very often/often having difficulty sleeping is equally likely among those in a couple (35%) as among single adults (36%) or those who are separated, divorced or widowed (35%).

Whether single or in a couple, anxiety and sleeping problems are reported more by women than by men
Previous studies of mental health have found that women are more likely to experience anxiety disorders and depression compared with men.2 This appears to be the case in a pandemic environment as well.
Women are far more likely than men to report very often or often experiencing anxiety during the coronavirus pandemic: almost 6 in 10 women who were in a couple (58%) or were single (59%)3 report feeling anxious or nervous very often/often, compared with fewer than 4 in 10 men who were either in a couple (37%) or single (37%) (fig. 2).
As for challenges during the night, more than 4 in 10 women report difficulty sleeping very often/often since the beginning of the pandemic, whether or not they are in a couple (44%) or single (44%). This compares with fewer than 3 in 10 men, whether in a couple (26%) or single (29%).
Single people are more likely to experience irritability and mood swings
Irritability and mood swings are more common among individuals who are currently single (fig. 1). Almost half of single adults (48%) report feeling very often/often irritable since the start of the pandemic, compared with 37% of those in a couple and 30% of those who are separated, divorced or widowed. Single adults (39%) also report mood swings in higher shares than those in a couple (31%) and those who are separated, divorced or widowed (27%).
Again, women, regardless of their marital status, are more likely than men to experience irritability or mood swings. About 6 in 10 single women (59%) and 42% of those in a couple report feeling irritable very often/often since the start of the pandemic. Men report being irritable very often/often in lower proportions than women, whether single (38%) or in a couple (32%) (fig. 2.).
Single women (46%) are the most likely to report mood swings very often or often since the start of the COVID-19 crisis, followed by women in a couple (38%). Men are less likely than women to report frequent mood swings, but those who are single (31%) tend to report mood swings very often/often in higher shares compared with men in a couple (23%).

Separated, divorced or widowed women most likely to feel sad
Feeling sad very often/often during the coronavirus crisis is more commonly reported among separated, divorced or widowed (51%) and single (48%) adults, compared with those in couples (43%) (fig. 1).
Frequently feeling sad is also more common among women, whether single (59%) or in a couple (53%) than among men, whether single (37%) or in a couple (33%) (fig. 2).
Mental health impacts the well-being of families
Mental health trends, by marital status and gender but also by other factors, will be important to monitor in the short, medium and long term of the COVID-19 pandemic. An initial analysis has shown that income or job loss and immediate financial strain also affect mental health symptoms, such as anxiety and difficulty sleeping during the pandemic. Furthermore, mental and physical health are linked – people with a mood disorder are at much higher risk of developing a long-term medical condition than are those without.4
Problems with mental health can have a serious impact on an individual’s education, work, social life and interactions with their family.5 Among Canadians who had at least one family member with a mental health problem in 2012, over one-third (35%) thought that their lives had been affected by their family member’s mental health and approximately 71% of those who perceived that their lives were affected by a family member’s mental health problem reported they had provided care to their family member.6
As such, the well-being of families in Canada is dependent upon on the mental health of the individuals who make up those families. Evidence-based decision making will better drive targeted social supports both for individuals and for families as the coronavirus progresses, as well as after the present crisis is over.
Ana Fostik, PhD, Vanier Institute on secondment from Statistics Canada
Jennifer Kaddatz, Vanier Institute on secondment from Statistics Canada
Notes
- A survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger, conducted March 10–13, March 27–29, April 3–5 and April 9–12, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. The March 27–29, April 3–5 and April 9–12 samples also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Caryn Pearson, Teresa Janz and Jennifer Ali, “Mental and Substance Use Disorders in Canada,” Health at a Glance, Statistics Canada catalogue no. 82-624-X (September 2013). Link: https://bit.ly/3btTtHk.
- Comparisons by sex are not possible for separated, divorced or widowed adults in this case due to low response counts.
- Patten et al. (2005). “Long-Term Medical Conditions and Major Depression: Strength of Association for Specific Conditions in the General Population,” Canadian Journal of Psychiatry 50:195–202 (2005). As cited on Centre for Addiction and Mental Health (CAMH), Mental Illness and Addiction: Facts and Statistics. Link: https://bit.ly/3eEjyWc.
- Mental Health Commission of Canada. Changing Directions, Changing Lives: The Mental Health Strategy for Canada (Calgary, Alberta, 2012). Link: https://bit.ly/2xEs4UI (PDF).
- Caryn Pearson, “The Impact of Mental Health Problems on Family Members,” Health at a Glance, Statistics Canada catalogue no. 82‑624‑X (October 7, 2015). Link: https://bit.ly/3bsRnaR.
Parenting in a Pandemic: A Story and the Stats
Jennifer Kaddatz
April 21, 2020
While trying to ensure that their children are safe, showered and schooled during the COVID-19 pandemic, many parents in Canada, as in other countries, are currently experiencing stress and sleepless nights. According to a survey conducted April 9–12, 2020,1 42% of surveyed adults living with children or youth said that they often/very often had difficulty sleeping since the start of the COVID-19 pandemic. I am one of those parents.
My own family includes three boys (pre-teen and teen), and soon I will be faced with a big credit card bill and some added stress, since the boys left their running shoes in their school lockers on March 12. Having worn boots to school that day, they now having nothing appropriate to wear on a warm Ottawa spring day.
My family has, so far, been extremely lucky in this pandemic. I continue to have a paid job and, like approximately 6.8 million Canadians surveyed by Statistics Canada in the last week of March (39%),2 I’ve been working from home, where it’s easier to avoid germs.
My parents and in-laws are living in isolation on the other side of the country, well cared-for within each of their relationships, like 81% of those in committed couples who say they and their spouse are supporting each other well during the crisis.3 My husband and I also count ourselves within the 79% of couples with kids at home who are supporting each other well during these unusual times.
For my family, the biggest ongoing stressor during the COVID-19 pandemic has, in fact, been related to school – or, more precisely, homeschooling. There are three generations of teachers on my maternal side, but I am not one of them. My boys are attending homeschool on their own for the duration of this pandemic. Elementary and secondary school teachers represent only about 2% of Canada’s labour force,4 which means that the rest of us are not likely qualified for the job.
According to Statistics Canada, 32% of Canadians are very or extremely anxious about family stress resulting from confinement due to the coronavirus.5 I can’t help but wonder what proportion of this anxiety is directly or indirectly related to the effort involved in trying to be a teacher, as well as a parent, while schools are closed.
Some families do not have the resources to enable stress-free homeschooling
Fortunately – or unfortunately, from the perspective of my 14-year-old son – a “pandemic” home education can now be delivered online in most parts of Canada. However, getting this education requires a) a stable, high-speed Internet connection with adequate bandwidth; b) access to a device or, preferably, multiple devices; c) a child who can focus, concentrate and be self-directed; or d) all of the above. The answer here is, of course, d). The question that remains is, therefore, “Is an online education achievable for children in all families across this country?”
A review of available data from official sources provides insight into the family characteristics that may result in greater challenges when it comes to obtaining an online elementary or post-secondary school education during the COVID-19 pandemic and, accordingly, where increased vulnerability might result in a long-term educational gap:
- Low-income households, rural households and Indigenous households are less likely to have the Internet access/speed required to complete online school activities at home. In 2017, only 24% of households in Indigenous communities and 37% of rural households had access to Internet at the minimum speed required to take full advantage of online opportunities, whereas 97% of urban homes had access at that speed or higher.6 In 2018, approximately 4% of households in the lowest income quartile did not have any Internet at home.7
- Low-income families are less likely to have a device other than a mobile device, which could make doing online school work challenging. Nearly one-quarter (24%) of households in the lowest income quartile reported using only mobile devices for accessing the Internet in 2018, three times higher than the share among households in the highest income quartile (8%).8
- Many families have more than one child who is required to complete school work at home, and yet the majority of households may not have enough devices to accomplish this easily. Close to 6 in 10 households (58%) that had Internet access as of 2018 had less than one device per household member.9 This figure was highest (63%) among households in the lowest income quartile.
- Like shoes, assistive devices may not have been sent home before schools were closed, which could impact the ability of children and youth with disabilities to undertake certain educational activities at home. Half of youth with a disability require at least one aid, assistive device or educational accommodation to follow their courses, according to the 2017 Canadian Survey on Disability.10
- Some children do not live in families were the environment is conducive to online learning:
- Almost 19,000 children were victimized by a family member in Canada in 2018 and in 59% of cases, the child was victimized by one of his or her own parents, who most often lived in the same residence.11
- Household food insecurity, which contributes to both poor mental and physical health, is when households cannot afford the quality or quantity of food needed for good health. Not surprisingly, data from 2017–2018 show high rates of food insecurity among households reliant on social assistance (60%) and Employment Insurance or Workers’ Compensation (32%).12
The statistics above only just begin to cover the myriad of intersecting barriers that can impede home learning, not to mention overall well-being, for families in Canada.
For many children and parents, school provides benefits over and above an education – benefits like social and emotional support, nutrition, increased physical exercise and a safe space to be themselves.
I, for one, have seen how many advantages my boys are missing out on since the start of the COVID-19 crisis just by virtue of the fact that they are no longer in school. And, as much as I love having them here at home with me, I cannot wait for them to go back.
Jennifer Kaddatz, Vanier Institute on secondment from Statistics Canada
Notes
- The survey, conducted by the Vanier Institute of the Family, the Association for Canadian Studies and Leger on March 10–13, March 27–29, April 3–5 and April 9–12, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. The March 27–29, April 3–5 and April 9–12 samples also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
- Survey data from Statistics Canada show that during the week of March 22–28, 6.8 million Canadians worked from home (39%), including 4.7 million who don’t usually do so. Link: https://bit.ly/2yqH9t1.
- April 9–12 survey by the Vanier Institute of the Family, the Association for Canadian Studies and Leger (see note 1).
- Statistics Canada, Occupation – National Occupational Classification (NOC) 2016 (693A), Highest Certificate, Diploma or Degree (15), Labour Force Status (3), Age (13A) and Sex (3) for the Labour Force Aged 15 Years and Over in Private Households of Canada, Provinces and Territories, Census Metropolitan Areas and Census Agglomerations, 2016 Census – 25% Sample Data, 2016 Census data tables, Statistics Canada catalogue no. 98-400-X2016295. (November 29, 2017). Link: https://bit.ly/2wSFdsD.
- Statistics Canada, “How Are Canadians Coping with the COVID-19 Situation?,” Infographics, Statistics Canada catalogue no. 11-627-M (April 8, 2020). Link: https://bit.ly/2wVzkuL.
- Minister of Rural Economic Development, High-Speed Access for All: Canada’s Connectivity Strategy, Innovation, Science and Economic Development Canada. Link: https://bit.ly/2XQNecT.
- Statistics Canada, Data to Insights for a Better Canada COVID-19 Pandemic: School Closures and the Online Preparedness of Children, Statistics Canada catalogue no. 45-28-0001 (April 15, 2020). Link: https://bit.ly/2zh73Qh.
- Ibid.
- Ibid.
- Statistics Canada, “Educational Experiences of Youth with Disabilities,” Infographics, Statistics Canada catalogue no. 11-627-M (September 10, 2019). Link: https://bit.ly/2RSInUN.
- Statistics Canada, Family Violence in Canada: A Statistical Profile, 2018, Statistics Canada catalogue no. 85-002-X (December 12, 2019). Link: https://bit.ly/2VlogAG.
- Valerie Tarasuk and Andy Mitchell, Household Food Insecurity in Canada 2017–2018, Toronto: Research to identify policy options to reduce food insecurity (PROOF) (March 2020). Link: https://bit.ly/3cFHDKB.
Canadians Turning to Their Screens to Keep Busy During COVID-19 Isolation
Jennifer Kaddatz, Ana Fostik, PhD, and Nathan Battams
April 17, 2020
In some ways, Canadians are making the best of their time in social isolation, according to four weeks of March and April 2020 survey data1 from the Vanier Institute of the Family, the Association for Canadian Studies and Leger.
As of the April long weekend (April 9–12, 2020), half of the country’s population aged 18 or older say they are relaxing “more often” now than they were before the pandemic.
Six in 10 adults are watching movies, television and videos or listening to podcasts more often than before the COVID-19 crisis started. Four in 10 are on social media more frequently.
More than 2 in 10 adults in Canada have increased the amount of time they spend listening to music, reading and playing games during the pandemic.
Half of adults are relaxing more, but some families report decreases in down time
Good news in these challenging times: people in Canada report that they are relaxing more.
Nearly half (49%) of Canada’s population aged 18 and older say that they are relaxing more often now than they were before the pandemic started, according to survey data from April 9 to 12, 2020 (fig. 1). Another 38% say that they are relaxing equally as often, while 13% say they are relaxing less often.
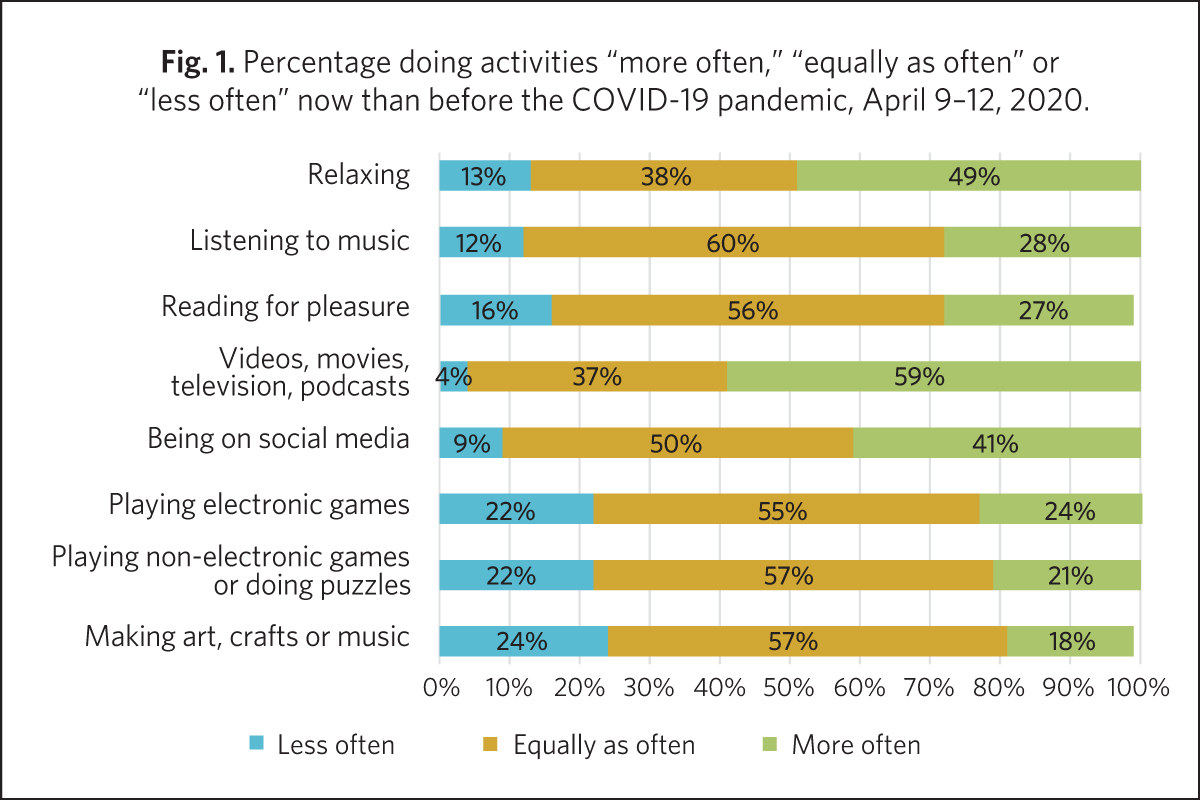
A slightly higher share of men (50%) than women (47%) report relaxing “more often” since the start of the crisis, with most of the difference attributable to younger adults aged 18–34: 64% of young adult males say they are relaxing more often since the start of the pandemic, compared with 56% of young adult females (fig. 2).
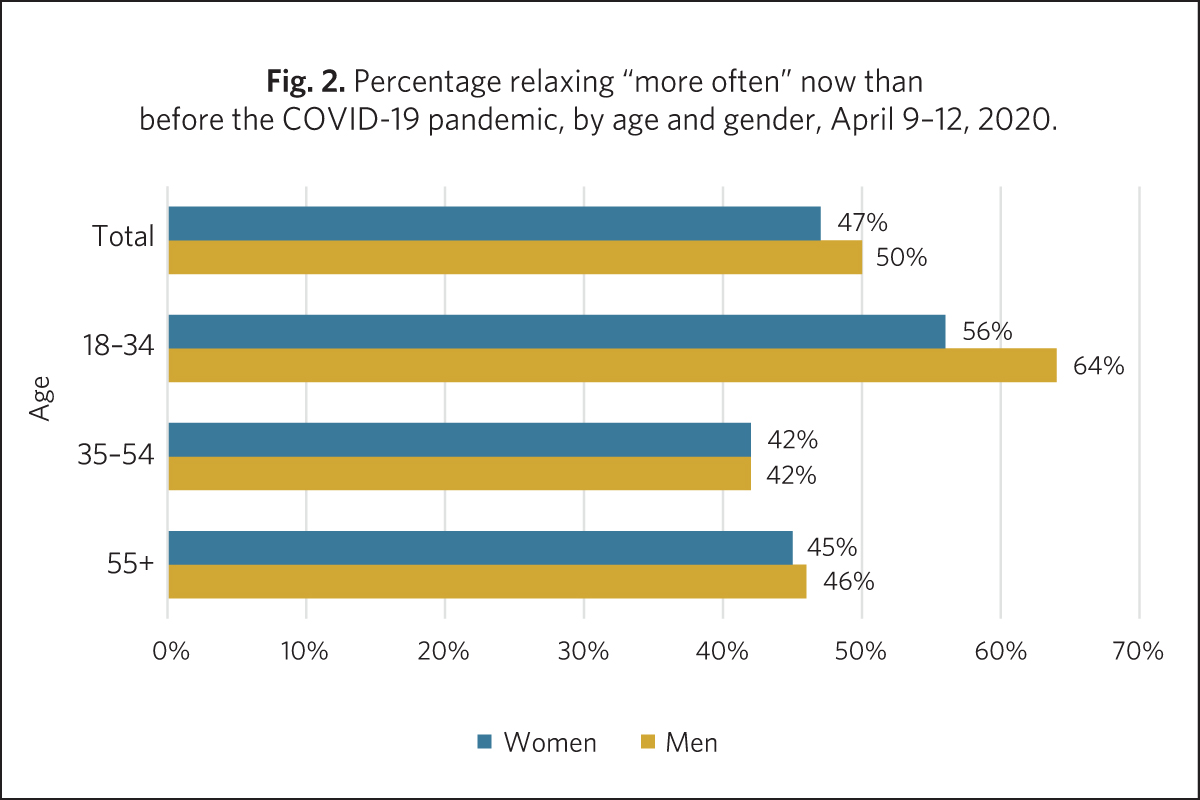
Perhaps not surprisingly, adults with young children at home (43%) are less likely than with no children or youth at home (48%) to say that they are relaxing more during the COVID-19 pandemic (fig. 3).
Almost 1 in 4 (24%) of adults who were living in the same home as at least one child under the age of 13 actually reported relaxing less often than before the crisis began.

Three in 10 are listening to music and reading for pleasure more often
About 3 in 10 adults in Canada are listening to music more often now (28%) than before the start of the COVID-19 crisis (fig. 1). This is similar to the share of those saying that they are reading for pleasure more frequently (27%).
According to an analysis of trends over time during COVID-19, there is a significant upwards tendency toward reading, with 23% of the population having said they were reading more often as of March 27–29 compared with 27%, who reported reading more often as of April 9–12.
Women are about as likely as men to spend more time listening to music (27% and 29%, respectively), but a larger share of women than men (29% and 24%) report reading more often since the start of the crisis.
Electronic- or screen-based pastimes are popular and show biggest increases in uptake
Survey data from April 9–12 show that many adults in Canada are turning to their screens to keep busy, as public health measures are keeping them at home.
Of all the activities for which adults were surveyed, “watching movies, television, videos or listening to podcasts” and “being on social media” had highest shares of adults, at 59% and 41% respectively, who say they do these activities “more often” since the start of the COVID-19 crisis (fig. 1).
The share of people saying they had increased the amount of time spent watching movies, television, videos or listening to podcasts was more than double the share of people saying they were reading for pleasure (27%) or listening to music (28%) more often now than in the past.
Furthermore, there appears to be an increasing tendency toward screens as the pandemic continues: 53% of adults in Canada had said they were watching movies, television, videos or listening to podcasts more often in week 2 of the survey (March 27–29) compared with 59% in week 4 (April 9–12).
The playing of electronic games also appears to be on the rise: 24% of all adults, or 26% of men and 22% of women, say that they are playing electronic games more now than they did before the pandemic started, according to the April 9–12 survey (figs. 4 and 5). These findings were similar to those published by Statistics Canada for the period of March 29–April 3, based on data collected in a web-based panel, which reported that 22% of all Canadians were now spending more time playing video games.2
Younger adults, especially men, have significantly increased the time they spend playing electronic video games since the start of the pandemic. More than half of men (54%) and one-third of women (36%) aged 18–34 report that they play electronic video games more often now than they did before (figs. 4 and 5).
As well, adults who had at least one child under the age of 13 living in their household (28%) were slightly more likely than those who had only teenagers at home (26%) and those who did not live with children at home (22%) to report playing video games more often since the COVID-19 crisis began.

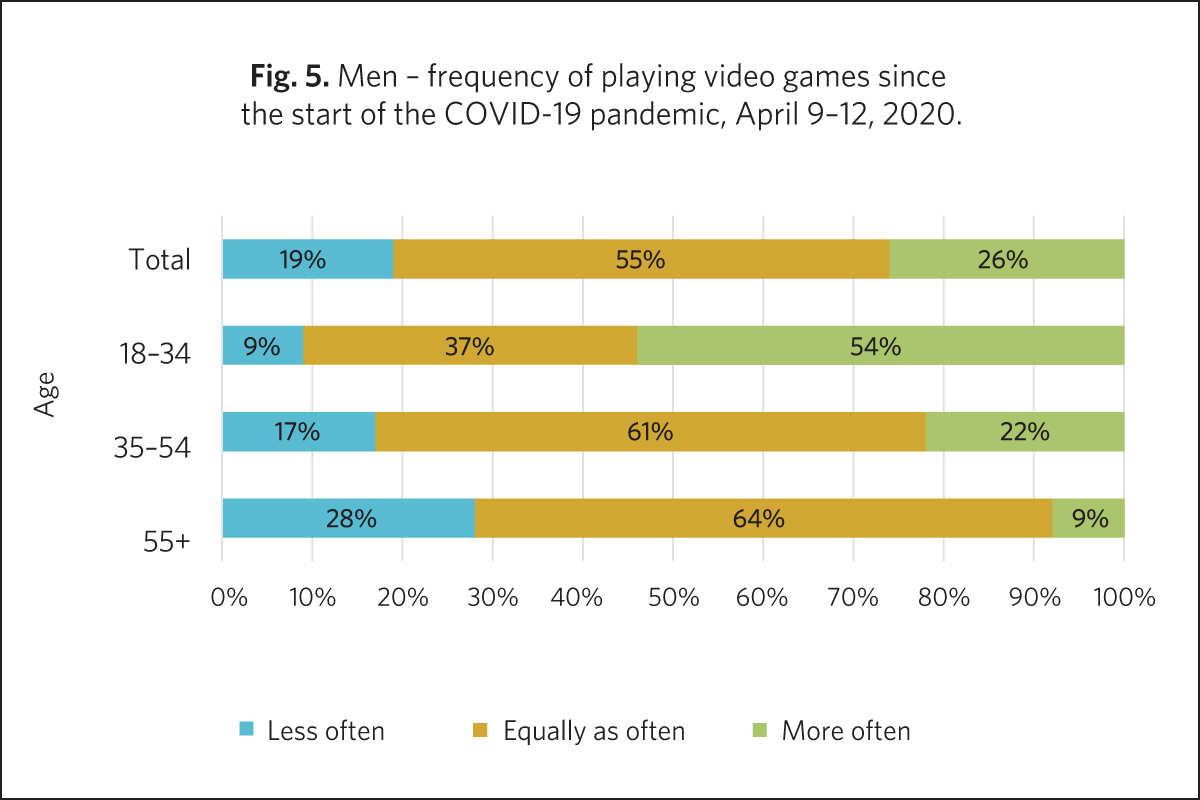
Women increase time playing board games and doing puzzles, men increase time playing electronic games
Despite the apparent popularity of screen time in general among adults in Canada, the share of those who report having increased their electronic gaming time since the start of the pandemic (24%) is only slightly higher than the share who have increased the amount of time they spend playing board games or doing puzzles (21%) (fig. 1). The share of adults who say that they now undertake these activities “less often,” at 22% and 22%, respectively, is also very similar. However, differences exist by gender and the presence of children and youth in the household.
Similar shares of women say that they play electronic games more often now than they did before the pandemic (22%) say they play non-electronic video games or do puzzles (23%). In comparison, for men there was an 8 percentage point difference in the uptake of the two pastimes, with 26% of men reporting they were electronic gaming more often now and 18% of men saying they were playing board games or doing puzzles more often now than they were before the pandemic.
Furthermore, a slightly larger share of younger women than men have increased the time they spend on non-electronic games or puzzles: about one-third of women (33%) and about one-quarter of men (27%) aged 18–34 report spending more time on this type of activity.
Relatively few older people in Canada report playing board games or doing puzzles more now than before the coronavirus pandemic: about 1 in 10 (9%) men aged 55 or older and 1 in 7 women (15%) of women aged 55 or older.
A significant proportion of women (54%) and men (55%) reported that they play video games “equally as often” as before the COVID-19 pandemic (figs. 4 and 5), though it is important to note that, in some instances, this could just reflect that they didn’t play video games to begin with.
Families with children more often play board games and do arts and crafts
Adults who had at least one child under the age of 13 living in their household (28%) or teenagers at home (22%) are considerably more likely than those who did not live with children (14%) to say that they have been playing non-electronic games and doing puzzles more often now than before the coronavirus pandemic started (fig. 6).
Furthermore, when young kids were in the house, adults are almost twice as likely as those with no children or youth at home to have increased their time spent making arts, crafts or music since the start of the COVID-19 crisis. As of April 9–12, 3 in 10 (31%) adults who lived in a home with at least one child under the age of 13 say that they have been making arts, crafts or music more often since the start of the pandemic, compared with 27% of those with only teenagers at home and 17% of those with no children under 18 at home (fig. 7).


Jennifer Kaddatz, Vanier Institute on secondment from Statistics Canada
Ana Fostik, PhD, Vanier Institute on secondment from Statistics Canada
Nathan Battams is the Communications Manager at the Vanier Institute of the Family.
Notes
1. The survey, conducted March 10–13, March 27–29, April 3–5 and April 9–12, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. The March 27–29, April 3–5 and April 9–12 samples also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20. Figures may not add up to 100% as a result of rounding.
2. Statistics Canada, “How Are Canadians Coping with the COVID-19 Situation?” Infographics, Statistics Canada catalogue no. 11-627-X (April 8, 2020). Link: https://bit.ly/2z6fm1g.
Survey Finds Gender Gaps in COVID-19 Pandemic Experiences and Responses
Jennifer Kaddatz
April 16, 2020
In a pandemic, as in life in general, women and men often have different experiences and behaviours. According to three weeks of survey data1 from the Vanier Institute of the Family, the Association for Canadian Studies and Leger, a higher proportion of women than men view the COVID-19 pandemic as a threat and have experienced physical, emotional and social impacts as a result of social distancing and home isolation.
- Women are considerably more likely than men to have experienced anxiety or nervousness, sadness, irritability or difficulty sleeping during the pandemic.
- Women are also more likely to follow safety precautions, say that they are satisfied with federal and provincial measures put in place to flatten the curve, and say that they would be accepting of more strict enforcement measures.
Women are more likely to view coronavirus as a threat but, over time, differences are converging
Women generally view COVID-19 as a bigger threat than men with regard to its impact on society. In the most recent cycle of the survey, conducted from April 3 to 5, 2020, a higher share of women than men say they perceive that the virus is a threat to the Canadian economy (94% vs. 91%), a threat to day-to-day life in their community (81% vs. 75%) and a threat to the health of the population as a whole (83% vs. 74%). Equal shares of women and men (53%) say in that COVID-19 is a threat to their personal financial situation.
When it comes to personal impacts on health,* too, women tend to express greater concern. Nearly seven in 10 (68%) of women aged 18 and older report that they are “very afraid” or “somewhat afraid” of contracting the coronavirus themselves, compared with 63% of men (fig. 1). Eight in 10 (80%) women are afraid that a family member will become sick compared with 73% of men.
When asked if they felt that the worst of the crisis was behind us, was now, or was yet to come, 69% of women say they feel that the worst is yet to come, compared with 64% of men. At the other end of the spectrum, 11% of women and 18% of men say they feel that the virus is not a real threat and is being “blown out of proportion”*; nevertheless, data for women and men over the past three weeks suggest that over time, these gaps have been converging (figs. 1 and 2).


The gender gap is more pronounced among young adults regarding relationships with family and friends
Data show that women and men in Canada have been working diligently to flatten the COVID-19 curve. Nearly 9 in 10 of women and men say that they practise social distancing, keep a safe distance of 2 metres away from other people, wash their hands more frequently than usual and only go out for necessities (fig. 3).
Little difference was found between women and men regarding reported shopping activities over the past week. Women are slightly less likely to have gone grocery shopping (69% vs. 72%), to a liquor store (13% vs. 17%) or to get take-out food from a restaurant (20% vs. 22%). However, there are bigger gaps in the shares of women and men who have been to a convenience store in the past 7 days (15% vs. 22%).

Larger gender differences are noticeable with respect to managing relationships with family and friends during the pandemic, especially when age is taken into account. Women were more likely than men to report that they have asked others to practise social distancing (86% vs. 79%), as seen in figure 3. The gender gap is most noticeable among women and men aged 18–24 (13 percentage point difference) but continues to exist on a smaller scale among those aged 35–54 (2 percentage point difference) and those aged 55 and older (8 percentage point difference), as seen in figure 4.
On the other hand, men – particularly younger men – are more likely to visit to friends and family during the COVID-19 pandemic: 30% of men aged 18–34 say they have visited friends or family since the start of the coronavirus crisis, more than double the share (14%) of women in the same age group and about four times the share of men aged 55 and older (8%) and women aged 55 and older (6%) (fig. 5).


Women are more accepting of potentially stricter measures to flatten the curve
Almost three-quarters of women in Canada (74%) are satisfied with the measures put in place to fight COVID-19 by the federal government, and 84% with measures put in place provincially, according to the April 3–5, 2020 survey results. This compares with 69% and 79% of men, and revealing a similar gender gap found in the March 10–13 cycle of the survey.
Women also more commonly report that they agree with potentially stricture measures which could be put in place to contain the COVID-19 pandemic. As of April 3–5, 7 in 10 (68%) of women totally agree that they would give permission for police officers to issue fines to citizens who do not respect the measures put in place, compared with 62% of men, and 49% of women and 46% of men would allow police to arrest people. If it came to a complete city quarantine, 43% of women say that they would totally agree with that measure, compared with 36% of men.
Higher shares of women experiencing anxiety, sadness, irritability and difficulty sleeping
Women are more likely than men to say that they have “very often” or “often” felt anxiety or nervousness, sadness, irritability or difficulty sleeping since the beginning of the COVID-19 pandemic. In fact, it is on these indicators where the greatest gender differences appear in the April 3–5 survey, with a 9- to 15-percentage point larger share of women compared to men reporting these experiences. (fig. 6).
Younger women, aged 18–34, are especially likely to report anxiety or nervousness “very often” or “often” compared with their male counterparts (63% vs. 40%), although they are also considerably more likely to report sadness (56% vs. 36%) and irritability (61% vs. 41%). Nearly half (45%) of 18- to 34-year-old females report difficulty sleeping, compared with fewer than 3 in 10 (29%) of men in the same age group.

Men feel closer to their partners but are also less likely to have someone they can count on in an emergency
Despite some gender differences in feelings and responses to the COVID-19 pandemic, women and men report in equal shares that they are managing life better (7%), about the same (65%) or worse (25% to 26%) than they were before the pandemic.
Interestingly, though, a higher share of men who are in a married or common law relationship say that the COVID-19 pandemic has brought them closer to their spouse (49%) and/or resulted in more meaningful conversations (52%), compared with women (41% and 49%).
When it comes to having someone to count on in an emergency, almost 9 in 10 women and men (85% of each) agree that they have people they can count on. However, 6% of men, compared with 3% of women, totally disagree that they have anyone they can count on in a time of crisis.
Jennifer Kaddatz, Vanier Institute on secondment from Statistics Canada
Download this article (PDF)
Notes
1. The survey, conducted March 10–13, March 27–29 and April 3–5, 2020, included approximately 1,500 individuals aged 18 and older, interviewed using computer-assisted web-interviewing technology in a web-based survey. The March 27–29 and April 3–5 samples also included booster samples of approximately 500 immigrants. Using data from the 2016 Census, results were weighted according to gender, age, mother tongue, region, education level and presence of children in the household in order to ensure a representative sample of the population. No margin of error can be associated with a non-probability sample (web panel, in this case). However, for comparative purposes, a probability sample of 1,512 respondents would have a margin of error of ±2.52%, 19 times out of 20.
*Data on threats related to their own health, threats to the health of a family member and whether or not the virus is a real threat or being blown out of proportion exclude women and men who reported that they or a family member already has/had the virus or who answered “Don’t know” when asked the relevant threat question. (These people were included in the data for other survey questions examined in this report.)
In Conversation with Lisa Wolff, Director, Policy and Research, UNICEF Canada
Nathan Battams
Download In Conversation with Lisa Wolff, Director, Policy and Research, UNICEF Canada
November 20 is National Child Day and United Nations Universal Children’s Day, special observances commemorating the adoption of the UN Declaration of the Rights of the Child and the UN Convention on the Rights of the Child. For those who study, serve and support children in Canada, these observances provide an opportunity to recognize and celebrate the diverse and unique contributions of children to society while promoting and raising awareness about their well-being.
As the 60th anniversary of the UN General Assembly’s signing of the Declaration of the Rights of the Child and the 30th anniversary of the adoption of the Convention on the Rights of the Child, 2019 marks a special year for understanding children and youth. This understanding has been strengthened through the publication of Where Does Canada Stand?, the baseline report for the Canadian Index of Child and Youth Well-being.
Lisa Wolff, Director of Policy and Research at UNICEF Canada, recently joined Vanier Institute Communications Manager Nathan Battams to discuss this innovative and groundbreaking snapshot of child and youth well-being, its development and future directions.
How did the Canadian Index of Child and Youth Well-being come into being?
For decades, we’ve been tracking the state of children in Canada and around the world using population-level data to help understand where progress is being made on child and youth well-being, where challenges remain and where there might be no progress or things might be getting worse. This data facilitates the work of policy-makers, researchers, advocates and influencers in creating better conditions for children and youth to grow up in.
More than 30 years ago, UNICEF started the State of the World’s Children reports, which have been influential in terms of measuring child and youth well-being. Since then, there have been many “state of” reports on many different conditions that also use indicators and population data.
In more recent years, UNICEF started to focus on high-income countries as well and, in 2007, established an Index of Child and Youth Well-being, which brought together a number of indicators of how children in rich countries are doing in different aspects of life into one composite number and ranking. We’ve since published iterations of that. In the most recent, 2017 index, Canada ranked 25th of 41 countries in overall child and youth well-being.
Through this index, we discovered that Canada’s ranking among our peer countries – rich countries that have similar resources to spend on children and should therefore be getting reasonably similar outcomes and can be compared in regard to how they’re doing – is consistently in the middle and making very little progress relative to some other countries who were able to actually advance their standing over time.
This prompted us to question how some countries such as the United Kingdom were able to move up the rankings with a fair degree of speed and why we were stuck in the middle. At the same time, we were finding that many organizations were keen to use the UNICEF rankings in their own advocacy and in creating their own statistical dashboards for children and youth. For example, the Growing Up in BC project was inspired by the UNICEF Index.
We also recognized that Canada has data about children and youth that can’t be compared to other countries, because it’s unique to Canadian surveys, and that this rich data could provide additional valuable insight into what’s going on in children’s lives and how things are changing. There was already the example of the Canadian Index of Wellbeing, which does that at the general population level as well as compares how social progress relates to economic progress. So, we decided that we would create a Canadian Index of Child and Youth Well-being, inspired by the UNICEF model and the Canadian Index of Wellbeing – one that would bring together richer, focused data and insights about how children are doing and, if we could iterate the index over time, would look at progress and gaps.
The first thing we did was to assemble an advisory group. It was a large and diverse group that grew over the three-year period when we were developing the index. We started with around 40 advisors from across Canada – multidisciplinary, coming from research and government and community organizations from across the country, to ask them about their thoughts on what an index should do.
Our resulting vision has two purposes. First, we want it to serve as a communication tool for Canadian decision makers and influencers across the country – one that highlights how our youth are doing and identifies opportunities for change and progress. Second, by compiling diverse data points, not just in a dashboard but as a comprehensive view across different dimensions of children’s lives, we can look for patterns and focus on some of the big actions that could really “move the needle” on child and youth well-being and focus on what actions might actually address big gaps.
The index, therefore, takes a comprehensive view of childhood, one that isn’t based solely on the indicators that have mattered traditionally to adults (and are therefore more likely to be funded in population surveys), such as education outcomes and health status. Those things really matter to adults, and they matter to young people too, but what our advisors and what the youth themselves told us (because young people were an instrumental part of the index development process) is that their lives have a lot of other important aspects as well. For example, how much play and leisure time they have? How much do they get to participate in their families and in society? What relationships are important to them and how are they doing? How do they feel about school – not just in terms of grades, but about the experiences of school itself?
The index takes a comprehensive view of childhood, one that isn’t based solely on the indicators that have mattered traditionally to adults (and are therefore more likely to be funded in population surveys).
We settled on nine dimensions representing broad, conceptual aspects of children’s lives that are measured by a total of 125 statistical indicators. Although it’s a lot of indicators, this approach provides a more comprehensive view of their well-being, and by organizing them into dimensions, we’re able to define child and youth well-being in a broader way and elevate some things that are important to young people as well as to some of the adults who were involved in the project.
The process to get there brought together several strands of inquiry. We looked at how others were creating indices and measuring child and youth well-being in Canada and around the world. We did a scan of practice, exploring some of the innovative and exciting approaches being taken, as well as some of the things that were already agreed upon that were important to measure and were validated in the research. We explored a lot of the literature, including research and knowledge brought into the development by our advisors, and we incorporated the lived experience of young people by asking them what’s important in their lives. A prototype of the index was created, which we brought back to young people to ask what they liked about it, what we were missing and what was problematic about our approach – it was an iterative process.
In some cases, the views of adults and youth clashed, and when this occurred, we let the young people decide. Family meals came up as an example. Some of the indicators you often see cited when people are talking about youth health ask if they have regular family meals. We know through research that has been validated, that young people who tend to eat more meals with their families often have a better sense of belonging, better mental health, fewer risk behaviours and better grades.
In some cases, the views of adults and youth clashed, and when this occurred, we let the young people decide.
But in talking to young people – and we made sure we talked to those furthest from opportunity, including First Nations communities and youth in closed custody facilities, where youth often have severed relationships with their families – many told us that family meals feel a bit too normative, are stigmatizing and made them feel badly about their lack of family relationships or otherwise weren’t realistic. This was true even for some in higher-income families, in which we heard statements such as “We don’t do that, we’re too busy.” Instead, we focus on measuring the outcomes – Are kids healthy? Do they feel they belong? – and less on what contributes to that. We can explore that in other ways.
Another clash was around the importance of pets. A research expert might say, “Well, pets were never really studied as important to well-being,” though there’s some emerging evidence in some other countries. But time and time again, when you ask young people about the important relationships in their lives, they go beyond what research has focused on in terms of parents, teachers, peers and other supportive adults in the community.
Time and time again, when you ask young people about the important relationships in their lives, they go beyond what research has focused on.
The children frequently made statements such as my pet is what makes me feel good, my pet is one of the primary relationships in my life. So, we included an indicator for it, because we want to track it over time to see how many youth are caring for pets and have this important relationship in their lives. Their pets can become important to stave off loneliness and to create a sense of acceptance. It may be that pets become more important as an indicator when other relationships are more difficult. It was something interesting that we heard way too often to omit – so it’s included in the index to honour that.
What did your team do to ensure that diverse experiences were captured, such as those of Indigenous children or immigrant youth?
Predating the development of the index, we held a series of roundtables, similar to the Vanier Institute’s Families in Canada Listening Tour events, with child-serving organizations and leaders. One roundtable was focused specifically on Indigenous organizations and leaders. We asked the question “What does well-being mean to you?” to get a community definition, since there is no single, official definition of well-being. That really centred the kinds of things we chose to measure.
There was also a lot of diversity in the advisory group, and not just in terms of culture, age and social and economic location in Canada, but also in disciplines and academic approaches.
From Indigenous leaders, we heard about the importance of access to culture and the integrity of the ecosystem and environment in all their relations around children and youth. So that shows up in the index in a dimension called Are we connected to our environment?, which was actually a fairly uncommon inclusion in measuring child and youth well-being, and there are measurable climate-related indicators such as exposure to air pollution and access to natural spaces. That environmental sensibility didn’t surface at any of the other roundtables – only the Indigenous perspectives. It’s also validated by the Sustainable Development Goals (SDGs), which we also measure in the index with indicators that are aligned to the child-focused SDGs.
There was also a lot of diversity in the advisory group, and not just in terms of culture, age and social and economic location in Canada, but also in disciplines and academic approaches.
What are the next steps, and what is your vision on how the index will be used?
We would like to see governments at the provincial, territorial and federal levels track a broader set of indicators and dimensions of children’s lives and focus just as much on things like their freedom to play and participate as we currently do on academic performance and drug use. Better benchmarking and monitoring of the state of children and youth can help guide decision makers and policy-makers with evidence-based insights.
In fact, the index is already being used, for instance, in the Region of Waterloo, which comprises a number of municipalities and rural communities. They voted on a new set of goals for children in the region aligned with the nine dimensions of the index, to broaden the scope of their focus and progress at the regional level. There are hundreds of organizations that come together in a child and youth planning table in the region and work together on providing services for children and informing policies, and this provides them with a wider lens.
Partners such as the Ontario Trillium Foundation are working with us to create a local survey tool aligned with the index. Any community could implement this survey to gather data about children and youth, which is really hard to come by on a local scale. This data tends to be missed in the big national surveys, either due to being overlooked entirely or because the sample size is too small. If communities choose to, they could benchmark how their youth are doing against other communities or against the national averages.
Better benchmarking and monitoring of the state of children and youth can help guide decision makers and policy-makers with evidence-based insights.
The Foundation of Greater Montreal has already started to do that. For instance, they created a Montreal-based report on the state of children using the UNICEF index of well-being in 2017, and they found that they were lagging behind the national average on food security. As a result, that has localized greater attention and more programs, and efforts are under way to address food and security in the region.
So these are some of the ways UNICEF’s data and analysis are being used across Canada, and we’re glad it’s resonating and opening new ways of thinking about ourselves, because this wider and more comprehensive lens on children and youth can facilitate and strengthen policies and programs to have a significant impact on well-being for children and youth across the country.
Lisa Wolff is Director of Policy and Research at UNICEF Canada, where she promotes public policy and practices that align with the principles and standards of the UN Convention on the Rights of the Child. Lisa leverages UNICEF’s global strengths, including data and innovation, and works across sectors with diverse partners to advance the rights of children in Canada – work for which she received the Queen Elizabeth II Diamond Jubilee Medal in 2012.
This interview has been edited for clarity and length.
Facts and Stats: Maternal Mental Health in Canada
Download Facts and Stats: Maternal Mental Health in Canada
Maternal health and well-being is an important public health issue, of which mental health is a key component. Data shows that while most new and expectant mothers report good mental health and high life satisfaction, experiences of postpartum depression (PPD) and anxiety are common in Canada.
Research shows that PPD and poor mental health are detrimental to the well-being of mothers and can, if left untreated, adversely affect infant development (e.g. low birth weight, preterm birth, increased risk of mental health problems in the child later in life), as well as leave partners and other family members (including fathers, who are at an elevated risk for depression or anxiety) feeling overwhelmed.
Fortunately, multiple effective and well-researched treatment options are available to help women recover, and research shows that social and emotional support from partners and other family members throughout the perinatal period can reduce the likelihood of PPD and emotional distress for both mothers and newborns.
This edition of Facts and Stats explores the mental health of new and expectant mothers in Canada, with a focus on family well-being.
Highlights include:
- In 2018–2019, most (60%) mothers who recently gave birth rated their mental health as excellent or very good, while nearly one-quarter (23%) reported feelings consistent with PPD or an anxiety disorder.
- In 2018–2019, 30% of mothers who recently gave birth under the age of 25 reported feelings consistent with PPD or an anxiety disorder, compared with 23% among those 25 or older.
- In 2018–2019, nearly one-third (32%) of recent mothers who reported feelings consistent with PPD or an anxiety disorder said they have received treatment for their emotions or mental health since the birth of their child.
- Maternal mental health is affected by socio-economic status, with research showing higher rates of PPD and depressive symptoms among mothers from marginalized groups, including people living with disabilities; recent migrant mothers, asylum-seekers and refugees; and mothers self-identifying as Black or First Nations.
- Mothers with adverse life experiences are also at a higher risk of developing mental disorders, such as those living in food-insecure households or in emergency or conflict situations, and those who have experienced violence (domestic, sexual or gender-based) or natural disasters.
Download Facts and Stats: Maternal Mental Health in Canada
This resource will continue to be updated as new research and data emerges (previous versions will be continually available on our fact sheets page).
Source information available on the PDF version of this resource.
In Focus 2019: Food Insecurity in Canada
Food insecurity in Canada is an issue deeply intertwined with the health and economic well-being of families. While there is no single cause for food insecurity, research shows that both economic insecurity and geographical isolation (in particular, the higher food costs in Northern communities resulting from a lack of year-round rail, road or marine access) contribute to families not having access to sufficient, safe and nutritious food to meet their dietary needs for a healthy life.1
Food-insecure families are more likely to experience adverse effects to their health and well-being, which include restricted mobility and chronic conditions, poor mental health and mental distress.2 This impacts individuals, families and communities, and incurs considerable costs on the health care system – it’s a matter of family well-being and public health.
In recognition of Hunger Action Month, which raises awareness on national, provincial and local levels about hunger in Canada, this edition of In Focus highlights data on food insecurity across the country.
Many Canadians – including children and youth – continue to experience food insecurity
- In 2018, 1 in 4 children and youth under 18 (23%) say they go to bed or school hungry at least sometimes because there is not enough food at home.3
- In 2018, children and youth under 18 accounted for 20% of the population in Canada but 35% of those who accessed food banks in March of that year.4
- In 2015–2016, approximately 16% of households in reporting provinces and territories across Canada5 experienced food insecurity.6
Northern populations and marginalized groups experience disproportionately high rates of food insecurity
- In March 2018, six in 10 people who accessed food banks (59%) were on social assistance or disability-related supports.7
- In 2015–2016, more than half (51%) of households in Nunavut were food insecure – by far the highest rate in Canada and more than three times the average rate of the remaining reporting provinces and territories (11%).8
- In 2015–2016, nearly three-quarters of the children in Nunavut (72%) and one-third of the children in the Northwest Territories (32%) lived in food-insecure households, compared with 16% to 23% among the remaining reporting provinces and territories.9
- Despite the launch of Nutrition North – a food retail subsidy designed to improve food access and affordability in isolated communities – annual rates of food insecurity actually increased in Nunavut between pre-implementation (33% to 40% between 2007 and 2010) and the years following implementation of the program (46% to 56% between 2013 and 2016).10, 11
- Research from 2014 showed that rates of food insecurity among Black people (29%) and Indigenous people (26%) were more than twice as high as the national average (12%).
Data gaps leave us without a clear picture of the prevalence and impact of food insecurity among diverse groups
- The Canadian Community Health Survey (the main source for information on food insecurity in Canada) doesn’t collect data from First Nations reserves, resulting in approximately half of all status First Nations peoples (approximately 300,000) being left out of the picture, and thus underestimating the prevalence of food insecurity.12
- Other diverse groups, including full-time members of the Canadian Armed Forces, people living in institutions and the 235,000 Canadians who experience homelessness in any given year are not represented in national food insecurity data (despite the latter being more vulnerable to food insecurity than the general population).13
Notes
- Paula Arriagada, “Food Insecurity Among Inuit Living in Inuit Nunangat,” Insights on Canadian Society, Statistics Canada catalogue no. 75-006-X (February 1, 2017). Link: https://bit.ly/2maW9oN.
- Ibid.
- UNICEF Canada, Where Does Canada Stand? The Canadian Index of Child and Youth Well-being: 2019 Baseline Report (September 3, 2019). Link: https://bit.ly/2kpOeDv.
- Food Banks Canada, Hunger Count 2018 (February 5, 2018).
- Newfoundland and Labrador, Ontario and Yukon opted out of food insecurity measurement in 2015–2016.
- PROOF Food Insecurity Policy Research, Latest Household Food Insecurity Data Now Available (June 25, 2018).
- Food Banks Canada, 2018.
- PROOF Food Insecurity Policy Research, 2018.
- Ibid.
- Research suggests this may be the result of the program’s focus on perishable, nutritious foods, as well as the exclusion of most non-perishable foods and all non-food items from the subsidy.
- Andrée-Anne Fafard St-Germain, Tracey Galloway and Valerie Tarasuk, “Food Insecurity in Nunavut Following the Introduction of Nutrition North Canada,” Canadian Medical Association Journal, 191:20 (May 21, 2019). Link: https://bit.ly/2m5FJhb.
- PROOF Food Insecurity Policy Research, Household Food Insecurity in Canada: A Guide to Measurement and Interpretation (November 2018). Link: https://bit.ly/2kAs2qd.
- Ibid.
Facts and Stats: House, Home and Family Finances (2019 Update)
Home is at the heart of family life, the primary setting in which our family relationships are built and nurtured throughout our lives, and the stage on which so many of our family memories are created.
Our relationships with our homes are shaped by the evolving social, economic and cultural contexts in which we live, and where we choose to call home can change over time as we adapt our expectations and aspirations to these ever-changing environments.
To further explore the relationship between families and their homes, we’ve updated our House and Home in Canada fact sheet with new data, this time with a focus on family finances and home.
Highlights include:
- In 2016, median monthly shelter costs in Canada were $1,130 for owned households and $910 for rented households.
- In 2016, 16% of owned and 40% of rented households in Canada had monthly shelter costs considered not affordable.
- According to recent estimates, it now takes 13 years for a typical person aged 25 to 34 to save a 20% down payment on an average-priced home in Canada, compared with 5 years in 1976.
- Recent estimates show that a typical person would have to earn at least $22.40 per hour to be able to afford renting an average-priced two-bedroom apartment in Canada.
Download the House, Home and Family Finances (2019 Update) fact sheet.
This resource will continue to be updated as new research and data emerges (previous versions will be continually available on our fact sheets page).
Published on August 15, 2019
Research Recap: School Experiences of Children in Military Families
Emily Beckett
Download Research Recap: School Experiences of Children in Military Families
There are more than 64,000 children growing up in military families in Canada.1 Many of these children experience high mobility, as studies show that military families move three to four times more often than their civilian counterparts.2 While most military families are highly adaptive and resilient during relocations, a growing body of research has found that these frequent moves can have an impact on family well-being.3
Nearly three in 10 surveyed military spouses (27%) report they have been relocated at least four times due to military postings.4
While frequent moves can affect multiple aspects of family life, some research suggests that the greatest disruption on youth is related to school and school-related activities.5 Parents in military families are aware of these disruptions, with more than half (54%) of surveyed military spouses agreeing that “military children are at a disadvantage because civilian public schools do not understand military life.”6 However, research also shows that a child’s school environment can facilitate the transition and have a positive impact on the well-being of youth in military families.
In recent review of available literature, School Participation and Children in Military Families: A Scoping Review, Heidi Cramm, PhD, and Linna Tam-Seto, PhD(C), explored existing research on how transition affects the well-being of children and youth in military families with regard to school participation. Through an examination of 112 academic articles, they found that experiences common in military families, such as separation from a deployed parent, relocation, parental deployment in dangerous conflict situations and changes to family dynamics during and after deployments, can all shape the quality and quantity of children’s participation in school-related activities. While the vast majority of the articles in the literature review are based on U.S. data, military families in Canada seem to share many of the same experiences and concerns, as reflected in data from the Canadian Armed Forces (CAF) Community Needs Assessment: 2016 Overall Results report.7
Resettling into a new community takes time
While starting at a new school doesn’t necessarily mean a child from a military family will experience academic difficulties, research in the literature review suggested that it takes students approximately four to six months to academically re-establish themselves each time they move. Though this period is temporary, these disruptions can have a long-term effect on opportunities later in life, specifically in regard to a child’s willingness to take risks or pursue challenges.
Based on the predominantly American research, Cramm and Tam-Seto noted that difficulties in transition among students were found to be associated with the duration of deployments (total number of months that the child’s parents are away on deployment), the mental health of the non-deployed parent and decreasing resiliency. Research also acknowledges the potentially difficult period of reintegration of a military member into family structures and routines after their deployment. Given that there is some evidence that the accumulation of months deployed is associated with these types of negative effects, it will be critical to determine what the experience is for military families in Canada.
Academic experiences and access to supports can be impacted by military life
Cramm and Tam-Seto found that students in the research, who were primarily from U.S. military families, can experience negative impacts on their academic performance (e.g., academic gaps and redundancies) when they move across jurisdictional boundaries: factors such as standards, credit requirements and the age of kindergarten can change from region to region. They also found that stress at home during deployment and reintegration can often affect in-school behaviour and class dynamics, as these students may act out emotionally and experience difficulties with concentration, anxiety and conflicts with peers. Though the survey doesn’t specify whether the problems exhibited in the children of the respondents to the CAF Community Needs Assessment were associated solely with mobility, 13% of respondents reported that their child exhibited emotional or behavioural problems at school in the past year. Further research is needed to provide a greater understanding and focus on military families in Canada.
In 2016, more than 1 in 7 surveyed CAF members (13%) reported that their child exhibited emotional or behavioural problems at school in the past year.
Studies found an association between behavioural and emotional adjustment and academic performance (e.g., conduct, attendance, attitudes toward school and approaches to learning). The difficulties associated with transitioning to a new school can be compounded when a student requires access to special education resources.8 Many of the 8.2% of surveyed CAF families who report having children with special needs9 require access to resources and supports, and the process of accessing them can be disrupted with every move.
Like any family with a member with special needs, many military parents of children with autism spectrum disorder (ASD) can face difficulties navigating health care and education systems, not only to acquire appropriate resources but to secure assessments and diagnoses as well.10 Obtaining a diagnosis can be difficult as families can spend months or even years on a wait-list, which can result in military families relocating before they receive care or services.
Many special education resources cannot be accessed without a diagnosis, and Cramm and Tam-Seto found that schools may delay providing resources based on the assumption that a student’s academic struggles are related solely to military life or a temporary reaction to a deployed parent. Alternatively, special education resources are occasionally provided rather than taking the larger step of addressing gaps in education due to relocation. Many U.S. school staff report that they feel unable to appropriately identify students in military families for clinical referrals.
Building community in the face of high mobility
Research shows that in the context of high mobility, military students can experience difficulties initiating and maintaining meaningful personal relationships and building social circles with children their age. Many civilian peers may not understand or be able to empathize with parental deployment or frequent moves, which can have an impact on relationships with military children. Social connections between military and civilian youth are common, since 85% of military families in Canada now live off-base in civilian communities, compared with only 20% in the mid-1990s.11
Cramm and Tam-Seto found that children of military families living in U.S. civilian communities are particularly vulnerable to feelings of isolation and loneliness – important measures, since the connection between strong social networks and well-being has been well established in research.12 Conversely, research shows that a sense of community belonging can be a factor in protecting mental health and enhancing resiliency.13
Participation in extracurricular activities can be affected by mobility among youth in military families. For example, opportunities for a child in a military family to sign up for a soccer team may have passed by the time they move, as the tryouts may have already been held and the team was set before the beginning of the academic year. Higher levels of sports teams or leadership programs may pass over military students to avoid complications that could arise if the student needs to relocate again.
The 2016 CAF Community Needs Assessment report found that among respondents who cited their child’s well-being as the most significant problem in the past year, nearly three in 10 (29%) reported requiring help with activities (e.g., bolstering fitness, stress relief, family bonding) to aid in the child’s well-being. Circumstances may not allow a parent to organize transportation to extracurricular activities or manage without the student’s support at home due to increased child care responsibilities during parental deployment, as 23% of all respondents reported experiencing issues with child care, such as quality, distance, expense and hours of availability.
Educational professionals have unique opportunities to facilitate transitions
Research suggests that teachers, counsellors and other educational professionals have unique opportunities to facilitate transitions for military youth. American research in the review suggested that the school environment can act as a protective factor during relocation, and that educators can support students in military families by strengthening the child’s resiliency and adaptive coping skills.
Due to the inherently disruptive nature of relocation and the potential loss of stability and routine in their lives, military families and students can be particularly reliant on school personnel and structure for social and emotional support. Among surveyed CAF parents who selected child well-being issues to be the most significant problem in the past year, more than one-third (34%) reported requiring emotional or social support. When families are able to get involved in their child’s schools, studies suggest it can enhance school engagement, academic success and their likelihood of graduating and pursuing post-secondary education.
However, Cramm and Tam-Seto also found that many U.S. educational staff report feeling overwhelmed by the magnitude of their students’ needs and struggle to deal with military family-specific issues, such as repeated transitions, parental deployment, fear of death or injury of a deployed parent, and how to meet those needs and communicate effectively with military families.
While many of the studies and research explored and cited by Cramm and Tam-Seto were from abroad, the findings are important in better understanding military families in Canada, who share many of the same “military life stressors” as their American counterparts – in particular, high mobility, frequent periods of separation and risk.14 The research in this scoping review study suggests that schools and educational professionals with a high degree of military literacy (awareness of these stressors and military family experiences) can play a major role in facilitating transitions among youth. Canadian-specific research with school communities will be important in the coming years.
Resources and information facilitate support for military youth
Enhancing military literacy among educational professionals can play an important role in supporting military youth and their families, and many have expressed a desire for resources to help them with this goal. Resources such as School Counsellors Working with Military and Veteran Families, published in 2017 in collaboration with the Canadian Counselling and Psychotherapy Association and the Canadian Military and Veteran Families Leadership Circle, can play an important role in creating and strengthening “military-literate” teams of school counsellors (and their colleagues) in schools across Canada by providing information about the military and Veteran lifestyle and sharing tailored resources.
Military and Veteran families are strong, diverse and resilient, and they make unique and valuable contributions to communities across the country. Many experience high mobility, which affects the well-being of military-connected children and youth, and, in turn, on the well-being and operational effectiveness of serving CAF members.15 Enhancing understanding of their experiences and the “military lifestyle” among educational professionals and others who study, serve and support families will be key to ensuring that communities and workplaces are inclusive environments in which these families can thrive.
Read the full study:
Heidi Cramm, PhD, and Linna Tam-Seto, PhD(C), “School Participation and Children in Military Families: A Scoping Review,” Journal of Occupational Therapy, Schools, & Early Intervention (March 1, 2018). Link: https://bit.ly/2qiWfcU.
Download Research Recap: School Experiences of Children in Military Families
Emily Beckett is a professional writer living in Ottawa, Ontario.
Published on May 22, 2018
This article was reviewed by Col. (retd) Russ Mann, Special Advisor to the Vanier Institute of the Family and former Director of Military Family Services, as well as Heidi Cramm, PhD, and Linna Tam-Seto, PhD(C).
Notes
- Heidi Cramm et al., “The Current State of Military Family Research,” Transition (January 19, 2016).
- Kerry Sudom, “Quality of Life among Military Families: Results from the 2008/2009 Survey of Canadian Forces Spouses,” Director General Military Personnel Research and Analysis, Chief Military Personnel (August 2010). Link: http://bit.ly/2b8Hp3U.
- Learn more with A Snapshot of Military and Veteran Families in Canada.
- Sudom, 2010.
- Pamela Arnold et al., “Needs of Military-Connected School Divisions in South-Eastern Virginia,” Old Dominion University Center for Educational Partnerships (September 2011), link: https://bit.ly/2EQGs9F; Angela J. Huebner et al., “Parental Deployment and Youth in Military Families: Exploring Uncertainty and Ambiguous Loss,” Family Relations 56(2) (April 2007), link: https://bit.ly/2qT6zrH; and Kristin N. Mmari et al., “Exploring the Role of Social Connectedness among Military Youth: Perceptions from Youth, Parents, and School Personnel,” Child and Youth Care Forum, 39(5) (October 2010), link: https://bit.ly/2vm4aey.
- Sanela Dursun and Kerry Sudom, “Impacts of Military Life on Families: Results from the Perstempo Survey of Canadian Forces Spouses,” Director General Military Personnel Research and Analysis, Chief Military Personnel (November 2009). Link: http://bit.ly/1pbjBgC.
- Prairies Research Associates, CAF Community Needs Assessment: 2016 Overall Results (September 2017).
- Cramm, 2016.
- Heidi Cramm, “Health Care Experiences of Military Families of Children with Autism,” Transition (November 6, 2017).
- Cramm, 2017.
- Ibid.
- Maire Sinha, “Canadians’ Connections with Family and Friends,” Spotlight on Canadians: Results from the General Social Survey, Statistics Canada catalogue no. 89-652-X (page last updated November 30, 2015). Link: https://bit.ly/1waJ2MQ.
- Statistics Canada, “Community Belonging,” Healthy People, Healthy Places, Statistics Canada catalogue no. 82-229-X (January 2010). Link: https://bit.ly/2Jl4MmX.
- National Defence and Canadian Forces Ombudsman, “On the Homefront: Assessing the Well-being of Canada’s Military Families in the New Millennium,” Special Report to the Minister of National Defence (November 2013). Link: https://bit.ly/2q6hi2a.
- National Defence and Canadian Forces Ombudsman, 2013.
Family Perspectives: Death and Dying in Canada
Death is a natural part of life, but many Canadians are hesitant to have essential conversations about the end of their lives. The Vanier Institute of the Family seeks to change this with the publication of Family Perspectives: Death and Dying in Canada, a conversation catalyst intended to spark dialogue in households, workplaces and communities across the country by exploring death and dying through a family lens.
Family Perspectives: Death and Dying in Canada examines the evolution of death and dying in Canada across generations, the desires and realities of families surrounding death and dying, the role of families in end-of-life care and its impact on well-being. Through current data and trend analysis, interviews with caregivers and families, and reflections on hospice volunteering from author Dr. Katherine Arnup, this study discusses death and dying within the current and emerging social, cultural and policy landscapes.
Highlights:
– Hospice palliative care can play an important role in helping dying people and their families, yet most Canadians don’t receive any.
- Palliative care benefits up to 85% of dying people at the end of their lives.
- An estimated 16% to 30% of Canadians receive some form of palliative care, depending upon where they live.
- Three-quarters (74%) of surveyed Canadians report having thought about end-of-life care, but only one-third (34%) have actually had a conversation with a family member.
– Medical assistance in dying (MAID) is having an impact on the conversation on death and dying in Canada.
- Since June 2016, more than 2,600 people across Canada have obtained medical assistance in dying.
- More than one in eight seniors in Canada (12%) say they or a family member have talked to a health care provider about access to MAID.
– Death is becoming less taboo in Canada, thanks to care providers and community initiatives.
- Hospice staff and volunteers, death doulas and other end-of-life practitioners are providing diverse forms of support to many families in Canada, including facilitating advance care planning and discussions about end-of-life care, coordinating care and providing grief support.
- “Death Cafés” are helping people across Canada to gather and discuss their thoughts about death and dying.
“While many people are hesitant to talk about death and dying with their families and health care providers, some of the silence surrounding death and dying in Canada has been broken – a step in the right direction,” says Dr. Arnup. “Talking about death with family, planning for what we hope for and supporting others can help us to see that death is a natural part of life that is not inherently undignified, and to appreciate the present, thereby enriching our lives.”
“Birth and death are among the few universal family experiences,” says Vanier Institute CEO Nora Spinks. “Many Canadians and their families are hesitant to discuss death despite the importance of these conversations in providing and arranging for the care of loved ones at the end of life. It is our hope that Family Perspectives: Death and Dying in Canada helps to move the conversation forward as we recognize and celebrate National Hospice Palliative Care Week.”
Download Family Perspectives: Death and Dying in Canada
Published on May 7, 2018
Alan Mirabelli: Hub Hospice and the Palliative Care Experience
Alan Mirabelli was the Vanier Institute of the Family’s Executive Director of Administration, who retired in 2007 after more than 30 years of service. He was diagnosed with cancer the first time in 2015 and again in 2017. Throughout his treatment and following his terminal diagnosis, he continued to be of service, mentoring many emerging artists and seasoned photographers, community leaders and elected officials. His characteristic kindness, generosity and mentorship had a significant impact on many people across Canada and abroad.
Over the years, Alan gave countless presentations, keynote addresses and lectures, and he facilitated many workshops with diverse groups in hotel ballrooms, quaint retreats and boardrooms and conference rooms. His final presentation was hosted by Hub Hospice Palliative Care, a unique community-based hospice-at-home organization in Almonte, Ontario that Alan came to know, as a recipient of their caring and compassionate services. He spoke to a large audience of community members, academics, health care professionals, end-of-life service providers/volunteers and their families. You could hear a pin drop as people clung to his wise and perceptive words. Alan invited people to donate to Hub Hospice, and died only weeks after giving the presentation.
This article is based on Alan’s presentation, which has been edited for print.
Hello, how are you?
In the Maasai culture, the common greeting is quite different – and it leads to a different result. Their greeting is, “How are the children? Are the children well?” By paying close attention to greetings, you can learn a lot about what matters to a people. When you consider the Maasai greeting, there’s a vision in the culture that goes beyond today. It’s not just a casual, passing remark – it reflects a sense of care and a sense of direction for the culture’s future.
When you live in a culture in which you are truly vulnerable, where there aren’t systems of health care and they don’t have all the things we take for granted, this expression of care is from the heart. The answer they expect is that all of the children are doing well, not just some of the children.
I use that story to point out the difference in cultures where care is expressed daily, and people aren’t simply asking if the children are well. What they’re doing, in fact, is preparing the next generation to look after them when they’re old. It’s anticipating the needs; if you don’t acculturate the young people and society to be interdependent and of service, you might not have access to the things you need in your times of vulnerability.
I think it’s very appropriate to what I want to tell you today, because it’s why Almonte has become my home since 1981. I have felt the daily care and concern for the future. It’s different in Almonte. It’s developed in a manner that’s consistent with what I see in the Maasai and the question of the greeting.
This presentation was prepared by me at 3:00 a.m. this morning. There is a reason for that. Some of you know me personally, and you know what an incredibly positive journey I have been on since being diagnosed with cancer.
I have been filtering things so that they become meaningful to somebody else, to other people who have not had this experience themselves. From these notes, which are only eight pages, triple-spaced, I could talk for 10 hours about this community of Almonte and about the people who have supported me thus far and will continue to do so until the end.
On a personal note, if you hear a negative undertone anywhere in this presentation, it is an accident of a mind. It is because it is becoming fogged. This afternoon is really tough for me mentally. If you hear any negativity, discount it. My heart is 100% positive and enlivened by the emotions, which are felt with joy and gratitude.
“If you don’t acculturate the young people and society to be interdependent and of service, you get none of the things you require and need in your times of vulnerability.”
Now I was asked to introduce myself, and rightly so, because anything I’ve done professionally – the fact that I was doing A, B, C in the past, giving hundreds of speeches per year – doesn’t help here. This is the toughest one.
What makes this conversation – and it is a conversation – is that I’d really like you to interrupt and ask a question when it is appropriate for you to ask that question. It is the equivalent of you saying, “Are the children well?” This matters to me. I want to understand you.
What makes this a unique case? Well, it is a case of one, me. You can diagnose this old guy on your own. I am a single person. Most people who turn to hospice turn because spouses and family members need the support as they go through the process of watching somebody they care about die.
By the way, you will not hear, as much as I can help it, euphemisms come out of my mouth. You will not hear of someone “passing” here. You die – that’s it. Euphemisms keep us from focusing on what really matters; and we have a culture that will talk at length about children and how much goes into that end of life, but we never want to talk about the other side.
I knew this day was coming since March 11, 1948. I didn’t know how and when I would die, I just knew that one day I would. There it is.
The second reason I’d like to talk about this is I’ve had the luxury of time – and it is a luxury. To be told you have cancer and you have four to six months (now down to one), it gives me time to say thank you, and to not do all of the things that my head says I have to. It is lovely to see my lawyer here, because she took care of the logistics around death and dying in the first week after I received the terminal diagnosis. Now I can speak from the heart, which is the only thing that matters to me. It really is.
As I said, I’m a case of one. I’m a single person, and I’m male. Usually there are people who surround you during times of illness, such as a spouse, who provides support and helps arrange for care. I’m very clear about how I want to leave this earth. I needed to find the people who would help me get there in the manner that I chose, not in the manner in which they wished to impose upon me. Therein lies a very nice bridge in this community.
I knew Hub Hospice existed, but I had a completely false image of what it was. I thought it was bricks and mortar, and they parked me in there, and I’d live my last days there. It’s a far more intelligent system than that, for which I am grateful. It is just what I need. I want a chance to express my gratitude, to be able to say “Thank you.” I want a chance to encourage the development of this model of care further in ways that really are meaningful not only to me, but to the family I choose to define for myself.
The other thing that this journey has taught me is that with the help of the volunteers that I have – and I have unbelievable volunteers, they’re really friends on call; that’s the way I can describe them – the experience that you get, through no other way than by doing what they do, is not an intellectual exercise but very much an emotional one. From my point of view, because I’ve had the luxury of time and I have a very clear vision of how I want to leave, I could ask for what I wanted clearly.
“Euphemisms [about death] keep us from focusing on what really matters, and we have a culture that will talk about children and how much goes into the beginning of life, but we never want to talk about the other end of life.”
Choosing Love and Life
Now I want to talk about why that matters. Just because I’ve been diagnosed with terminal cancer doesn’t mean that I choose to stop living! I wanted to find volunteers who, if asked, would help me live – fully – not watch me die and hold my hand while I do it. That time will come, but that is not what I want right now. As some of you know, art and photography is a lifeline for me. It is a meditation. It is everything that feeds my soul. I wanted two people who, if I said, “Could you drive me somewhere,” would say, “What time?” And they both have.
If I need to go downtown because I want to get something from the store, even though I’m weakening, “What time and when?” You know, just getting that opportunity to nourish that little piece of me has done more to enliven me. These days are getting harder and harder, but both of the volunteers are interested in what I’m doing, so the conversations become real and not sort of passing time.
When I was clear in asking for what I wanted, they were able to respond in a manner that works for them and works for me, and I tell you, it is what keeps me going every day. Every day is a surprise and they’re part of it somehow. Whether it is anticipating the next visit, arranging the next visit or outlining what we might do – and it might have to change on that day because I’m not up to it – that possibility is so vital to me.
Life can be just two emotions: fear and love. The moment I got the diagnosis, I chose the latter. It could be morbid. Ultimately for me, choosing that was probably the wisest thing I could do because it led to an increased sense of spirit. The number of people who have texted me and emailed me and said, “You’re showing courage doing that.” I said, “There’s no courage involved. It is what I want.” It is who I am. Why should I change that?
Let me switch tracks for a minute. Some of you know that I used to work for the Vanier Institute of the Family as Co-Director with Bob Glossop: an incredible 30-year history. I thought a number of things had changed over those years, but either we haven’t perceived them or if we did perceive them, we have chosen to ignore them at our peril.
We’re making assumptions at the level of public policy when it comes to care, possibly at local policy, in the service sector, about who is home to look after people – anybody – and provide the care they need. If you think about families becoming smaller and the demands of the economy, a need has been created for community groups like Hub Hospice. This evolution in our families and communities wasn’t sudden.
These are changes that are continuing. The first institution in society that reacts to change is never government, it is never our public institutions – it is always family. If you can’t make ends meet at the end of the month, you do one thing and one thing only, you send another member of the family out to work. How many double-income families do we have here? A lot of them. Who is home to provide care? Grandparents now are active, and they are not necessarily available to provide care.
Finally, families in the 1940s had on average five people in the household, but this has since fallen to three and it continues to fall. For many single people, there’s really nobody available to provide care.
If you look at mobility rates (how often people move), 50% of Canadians move every five years between cities, actually between streets, cities, provinces, countries. Try that with a bush and see how long it survives. When there is no one, who do you call when you’re told you’re terminally ill? Who?
Well, my family is no different. I have one sister who lives five hours away and one son who has five children under 11 years of age. So the question is, how do I arrange for the things that I know I would need, when I know I want them in a particular manner so that I don’t become a victim of cancer?
In my case, I learned about Hub Hospice services that were available in in my community by accident. That’s why I offered to make this presentation: to help others learn about the exemplary services available. I heard about the hospice service and how it works; I chose to reach out and make contact because, for me, it was an element of hope.
“Life can be summed up in two emotions: fear and love. The moment I got the diagnosis, I chose the latter.”
Getting the News: “It’s Terminal”
I am going to stop here for a moment and describe what it was like to get the news that you have a terminal illness.
In April 2015, I was diagnosed with throat cancer. The oncologists in the medical system in general were superbly amazing. Everyone I met through my treatment showed me care and compassion.
The compassion part is what I was looking for. I don’t expect it from the medical system, as well organized as it is. This isn’t a blame game; there are simply too many patients, too many sick people, too many fears. There’s got to be some middle ground to transition to the human side. Then when you try to invoke it from the medical system, of course, you get their impatience, and I understand it. However, when you really need the health care system, it really comes through for you and there’s nothing better.
I was standing in the Mill Street Bookstore, talking to Mary (the store owner) when my cellphone rang. It was my family physician, who had received the radiology report. He asked if I could talk. It is not very often that you get a doctor calling you directly, and also hard to get them back on the phone, so I said yes as I stood in front of Mary. He told me that my cancer had metastasized and was terminal.
Mary knew something was serious, and she looked at my face with care and compassion. That look kept me grounded. Without knowing the details, she understood that something real and important had happened, so right there – in the community – that first moment of human connection made a difference that day and has ever since.
I thanked my doctor and I was taken aback for no more than 30 seconds – literally. It didn’t take any longer than that. It was: This is it… this is the road I am now on.
The metaphor I have used to describe this journey is my life being a run-on sentence. I do what I do, and I don’t give it much thought, because it is who I am. Then suddenly I got that call and it was like somebody put a comma in that sentence. That’s what I felt. In seeing that comma – which was my diagnosis – I was at a point of choice: What am I going to do after the comma and before the period? The choice took a nanosecond. It was that clear.
I then walked out the door and ran into a friend whom I knew through photography. He said, “You look a little white.” I said, “Well, I just got this news…” My fear of cancer just washed away. That point of choice was vital for me. For somebody else, it might take longer. But here was my concern, which had nothing to do with dying, end of life or my physical well-being: This will be a huge strain on my family. How do I manage that?That was my first reaction.
My second concern was that our health care system, as good as it is, has become so complicated. I had no idea where to start. I needed a navigator from the point of view of the system. I knew I needed help. But what I also knew was, and in my state, I’m a very emotional man by nature. I have no fears of expressing it. You’ll see me cry somewhere along the way. I’m very comfortable with that. But I was also concerned about where I would get the emotional support I needed without overtaxing the people in my life… my small, busy family… the people who care about me… the people who will be caring for me? Yet I knew that, if I was going to get through this with the joy and the sense of purpose that I have, I would need a circle of support around me.
“My life has been a run-on sentence… Then suddenly I got that call and somebody put a comma in that sentence… What am I going to do after the comma and before the period?”
What that led to was a question of how one prepares for death long before one faces it. I lived with depression throughout my adult life. Medication wasn’t the solution for me. So instead I took a year-long sabbatical and focused on developing a spiritual approach to my life, a life that you see in my photographs. My photographs are based on the beauty I see and the joy it brings to me. I share my images so they bring joy to others. It is a short way of saying how I have lived the last 20 years. I’ve chosen to live with daily meditations, focusing on meaning, creating meaningful relationships or receiving meaning by mentoring a sincere group of photographers who have given me purpose and joy in my life.
Jamming on the Brakes
I will give you some advice: don’t get involved in the love/fear debate, but develop an attitude and a set of actions that really do invite you in and provide clarity of what matters. My life was moving forward like everyone else’s, at considerable speed, when with that phone call from my doctor, it was like somebody had jammed on the brakes: the whole world continued to move forward, and I was right there at the windshield, stopped. It felt like I was pressed against this windshield and that I was alone. It is the aloneness that got me, and the burden that I’d become on others.
I can’t describe the aloneness because it is not loneliness. It is a wholeness that haunts. You want to say something to somebody because they mattered and yet you haven’t got the voice. You haven’t got the capacity to articulate something that is life-giving. It is a very strange feeling. Then I started to think, What if I were married? All of everything I’ve encountered as the patient has been absolutely superb. Absolutely superb! If I need something, I can probably figure it out. I can see if I can find somebody who can point me in the right direction.
I thought for that moment, at the windshield, that what I’m feeling has got to be better than what a spouse or family member is feeling, watching their relationship of a lifetime just fade into the haze in front of their eyes. Feeling that aloneness and that incapacity to make a significant difference beyond a certain point, I just couldn’t imagine.
Hub Hospice in Almonte: Authentic Kindness
 When I first learned about Hub Hospice in Almonte and its unique approach to hospice at home, I thought, Somebody really thought this through. They understood the experience of the family caregiver; they started there in the family and the home. They understood the patient, but they also understood the spouse.
When I first learned about Hub Hospice in Almonte and its unique approach to hospice at home, I thought, Somebody really thought this through. They understood the experience of the family caregiver; they started there in the family and the home. They understood the patient, but they also understood the spouse.
I cannot imagine the conversations around the boardroom table that developed the vision that created this unique hospice model. Having negotiated many a vision and tried to implement them, they can be a nightmare! There are competing interests, there are competing visions, there are the big bricks-and-mortar people, there are the little keep-it-simple people… there is a wide range. It is a palette. To find one that actually feels right and to fulfill it, I just thought, Wow.
What is unique about Hub Hospice is its focus on family. First of all, it started from the position of the spouse. Second, whatever arguments, and I’m sure they weren’t pleasant, that derived from this model, delivered so consistently… the compromise is elegant. I can’t say it any other way. There is a volunteer perspective that I now have come to respect and give that is based on kindness. It is authentic. It is a kindness that provides a very human foundation for what I’m going through and what I imagine a spouse would be going through.
I have two volunteers. Each has a personal style. What amazes me is how complementary they are. Let me describe to you a meeting that I convened in my home a few months ago. I brought my care team together to plan and prepare for my end-of-life journey and the living I want to do along the way. My team included my palliative care nurse (a hero in my books); my son; my power of attorney for personal care, who is the person who ultimately makes all of the decisions for me when I can’t; and my Hub Hospice volunteers. I sat at the head of my dining room table, and I felt like I was the chairman of my destiny because of who was present. When I got emotional – and I did because there was such kindness at that table – whenever an issue arose, the appropriate person had a contribution to make. The team had only respect for me and my wishes. That’s when the tears started.
To have a team, who didn’t know each other before the meeting, set aside the things that usually divide a group and focus on developing the care plan – and occasionally have a hand reach out and just hold mine with no words – that comes from this notion that we start from: kindness.
There were no competing interests; I trusted everything that was communicated. I had confidence that the journey would be as I wanted it to be, and everyone around the table agreed to work together to see that it did. That they could work so coherently together so quickly speaks volumes to everyone in the room. The way they treated my son, trying to hear and elicit his concerns, that was probably the most touching moment for me. In terms of how hospice acted, they were mandated to support me and my family in this manner.
“There is a volunteer perspective that I now have come to respect and give that is based on kindness. It is authentic.”
My biggest joy was when I first met with the staff person and, subsequently, my volunteers. One of the first questions in the interview that I asked with the volunteers and my staff person was who they would talk to and who they wouldn’t talk to. The response I got just made my heart burst, because they understood completely the modernity of life. Family is like an elastic band: it stretches, it contracts, depending on the economy, the culture and a variety of other things. For many now, particularly the young, they create their own tribe or family. They really do, and I have as well.
I can’t tell you how appreciative I am of the flexibility that allows me to define who is intimate, equal to a blood tie, because some blood ties are very messy.
I have assurance that the right people are looking out for me when I define who is “family” and who needs to be provided with the information. To have an organization willing to do that, it is what I want now – and that is what they provide. I have alluded to the fact that, for me, palliative care is not about death and dying: it’s about finding a group that will support life and living.
The Importance of Listening
I’ve just told you how much family means to me in terms of not just being limited by blood. Why? Because that’s how we form lasting relationships in this culture at this time. I certainly have. The reason I cherish the people who are part of the hospice, and I mean cherish, is because when I talk to them, first of all, they listen. They have probably the most acutely developed sense of being rather than doing. It is a rare commodity. Everybody shows up on my door wanting to do something.
What amazes me is that each Hub Hospice volunteer whom I have dealt with is perceptive enough to recognize that, and to make the space to be quiet when it’s necessary, to laugh when it’s important and to cry when it matters. When I say palliative care is what supports life and living, the people at Hub Hospice do it. When I ask for a perspective, a point of view because of their experience, I get clear responses to consider.
“Palliative care is not about death and dying: it’s about finding a group that will support life and living.”
I don’t get told what to do, I don’t get told how to do it. To have a palette – and some of it I refer to as my emotional guides, some of it I refer to as a topographical map that helps me navigate my day and the care I receive because I have no idea how to manage it all… I have never done this before! – to have people who have experience and the human side of attentiveness is what I cherish every day.
“Defining end of life care is… to make the space to be quiet when it’s necessary, to laugh when it’s important and to cry when it matters.”
Now I am going to change to another part of this: the palliative part of it that I’ve come to understand, unfortunately. You notice when you’re around young families who want to talk about education or you’re around young teachers who want to talk about education, they never talk about learning. They talk about money and unions and the board of education, but not learning.
It is the same when you try to form an organization of any kind. You define your end, but then you get a hundred reasons why you can’t do it. Maybe it’s that you don’t have enough money, that you have to go through this step, that step.
A Different Model of Palliative Care
The way Hub Hospice is modelled is brilliant. There is nothing that can’t be done because they’re not depending on grants or bricks and mortar – they are dependent on volunteers, who work to ensure that I’m where I want to be.
Where do I want to be? In my home with the things I adore, with the things that make me alive. To be removed from my home to go to a “hospice” or “day program” in the cold or extreme heat would be uncomfortable. But these wise people have adopted a system that is flexible, responsive and allows me to stay at home. What I’ve come to appreciate is that Hub Hospice has a model that supports human needs. They’re based on kindness, not on the currency of efficiency.
Each cancer patient is complex and receives care from a well-developed medical model in our publicly funded health care system. From my experience, all the techs, all the doctors, all the nurses are fantastic, but it’s patient-focused. Hospice is all about support and guidance for the family – the family as defined by the patient.
For families, it is asking the right questions at the right time. When I need help, whom do I call? Will it be given freely? Will it be given begrudgingly or generously? Those are the things that matter. Support for those who care is vital, and palliative care supports dying with dignity and grace, peace and joy, and love and care. That’s it for me.
Palliative care speaks to and supports those who care for the patients and who ultimately ease the anxiety of the patients – the family. As I’ve told you, my life has been a run-on sentence – and then comes the comma, a terminal diagnosis. I’m moving toward the period and the end of my journey is coming. I’ve chosen a path and I’m choosing to speak about it. I’m not battling anything. I’ve chosen to live fully until I can no longer do so with or without support.
Making Images Is Like Palliative Care
When I make an image, and most of you will know and have seen my images, I always stand behind the camera and the tripod for 45 minutes or more before I make the image, because that time is an invitation. A slight shift from here to there or from this position to that position changes everything. The whole interpretation changes – the whole meaning changes – the whole experience changes. It is that focus, positioning and patience that is crucial.
Hub Hospice is like the photographer in me. The organization and the volunteers stand there observing, waiting for 45 minutes or more to see if they need to make a slight adjustment in order to make a big difference for the patient and their family. I can’t think of a better metaphor, because, in my experience, it’s the small gestures that make the biggest difference.
“Palliative care speaks to and supports those who care for the patients and who ultimately ease the anxiety of the patients – the family.”
In this day and age, it is very hard to find volunteers who will do anything more than once – forget about doing something more than once, twice, three times over a month. To get somebody to commit for an indefinite period of time to care for someone is challenging, and for someone they don’t know seems impossible. Making that commitment is heroic on the part of the volunteer and speaks volumes about the organization. Volunteers don’t make their commitment alone; I find it incredible that there are families in this community that will support the volunteers to sacrifice a good part of their lives for an extended and indefinite period of time. That is a demonstration of how the community supports one another directly and indirectly, a fact I don’t take for granted for a minute. It is to be celebrated and to be honoured.
It leads to a more potent question: how did Almonte develop this kind of caring and compassionate culture? These things don’t happen by accident. I chose to live in Almonte in 1981 because it is a community I felt I wanted to live in. Partly because community matters to me and I really have a sense of what community means to me. I can honestly say Almonte is my home. Having lived in different countries, having lived in different cities, Almonte is my home. It is partly because of its scale, but also because of who chooses to live here, its history and its traditions.
This is what has made this experience so enlivening. It is not an accident, for me, that the hospice was therefore created as it was. First of all, you have a community that has a long history: where a lot of people didn’t move every five years, where families have deep roots, where those roots are visible and talked about. Stories are shared. When somebody like me comes in where families are scattered all over the world, I see them as kind of memories. Somebody mentions a name and somebody at the table will spend the next 20 minutes telling the family history. The fact that people here tell stories, stories about their history, their families for generations, that’s what it’s meant.
It’s not always cute, it’s not always nice and pleasant, but the roots are deep and they’re real. I, the city guy, don’t have to come in and do anything. I just have to absorb tradition. This is a traditionally rich area having large families. They are still in the area. They still talk to each other. They still make contributions. It is the stories we tell each other that remind us that we live in a community that has provided a solid foundation for places like Hub Hospice.
We have an incredibly well-educated community; the people who come from afar tend to want to stay. They’re here to absorb this tradition, understand it, feel it and see how modern culture can be fitted in so that Almonte keeps up but doesn’t lose its strength of tradition. That’s how I see the palliative care process having been formed. People at that table remembering how it used to be done, recognizing it can’t be done that way, but rather how it can be adapted within a legal framework and within compassionate frameworks. It has that think and feel. It is not make-believe. It is why I like what they’ve done with Hub Hospice.
“Almonte is my home. It is partly because of its scale, but also because of who chooses to live here, its history and its traditions.”
I may be making all of this up because this is a case of one, and you can’t generalize. But from a case of one, I’ll tell you it’s made a huge difference.
Today my state of mind may be very fogged, but my state of heart is clear as crystal. It really is. My state of emotions is high and comfortable. The emotions are about gratitude and appreciation for our community that is responsive and chooses to be caring and compassionate. I no longer worry. It has become a conversation that is evolving as it needs to, with comfort, dignity, respect, tenderness and I can’t think of enough words to express how it feels.
The decision I made to come here in 1981 is the best decision I ever made. The decision to say this is my home and to really believe it is the best decision I ever made. I can’t imagine going along this journey any other way but with the joy and gratitude that you’ve afforded me. To the board, to the staff, to the volunteers at Hub Hospice, I thank you. You’ve made the difference. Not just intellectually, but to the heart and to the soul.
I thank you for listening.
Download Alan Mirabelli: Hub Hospice and the Palliative Care Experience
Alan died on December 20, 2017, a few weeks after he gave this presentation at Hub Hospice Palliative Care. Along with family and friends, his Hub Hospice volunteers were with him as he took the last few steps on his journey. In his final days, every time he woke up he would say, “I am so lucky, I am so blessed, I am so grateful.”
Published on April 3, 2018 with permission from Alan’s family (Marilyn Mirabelli and Michel Mirabelli)
Photo (top of page) by Peter Waiser
Families in Canada Interactive Timeline
Today’s society and today’s families would have been difficult to imagine, let alone understand, a half-century ago. Data shows that families and family life in Canada have become increasingly diverse and complex across generations – a reality highlighted when one looks at broader trends over time.
But even as families evolve, their impact over the years has remained constant. This is due to the many functions and roles they perform for individuals and communities alike – families are, have been and will continue to be the cornerstone of our society, the engine of our economy and at the centre of our hearts.
Learn about the evolution of families in Canada over the past half-century with our Families in Canada Interactive Timeline – a online resource from the Vanier Institute that highlights trends on diverse topics such as motherhood and fatherhood, family relationships, living arrangements, children and seniors, work–life, health and well-being, family care and much more.
View the Families in Canada Interactive Timeline.*
Full topic list:
- Motherhood
o Maternal age
o Fertility
o Labour force participation
o Education
o Stay-at-home moms
- Fatherhood
o Family relationships
o Employment
o Care and unpaid work
o Work–life
- Demographics
o Life expectancy
o Seniors and elders
o Children and youth
o Immigrant families
- Families and Households
o Family structure
o Family finances
o Household size
o Housing
- Health and Well-Being
o Babies and birth
o Health
o Life expectancy
o Death and dying
View all source information for all statistics in Families in Canada Interactive Timeline.
* Note: The timeline is accessible only via desktop computer and does not work on smartphones.
Published February 8, 2018
Facts and Stats: Families and Mental Health in Canada
At some point, most families find themselves affected by mental illness, whether it’s because a family member (or multiple family members) personally experiences a mental health condition or because they’re providing care to someone else – or both. With appropriate treatment and support, however, most people who experience a mental illness will recover,1 and families often play an important role in providing, arranging or helping pay for care.
Our new fact sheet provides an overview of families and mental health in Canada, including rates of mental health conditions within families, factors that contribute to mental illnesses and the roles family members can play in mental health treatment.
Notes
- Centre for Addiction and Mental Health, Mental Illness and Addiction: Facts and Statistics (n.d.), accessed September 20, 2017. Link: http://bit.ly/2jLyV6Y.
Health Care Experiences of Military Families of Children with Autism
Download this article in PDF format.
Heidi Cramm, Ph.D.
Military families in Canada are highly mobile, relocating three to four times more often than their civilian counterparts.1 This mobility has been found to complicate access to health care for these families, most of whom live off-base (85%, compared with only 20% in the mid-1990s) and rely on provincial and territorial civilian health care systems. This has an acute impact on the 8.2% of military families who have children with special needs, including those living with Autism Spectrum Disorder (ASD).2
Autism Spectrum Disorder (ASD) is a common neurodevelopmental disorder with an estimated prevalence of 1 in 68 children. While this condition primarily affects social communication, often making it difficult for people living with ASD to share enjoyment or emotional experiences with others, it has a range of symptoms and associated behaviours:
- Approximately 25% of people living with ASD are non-verbal, unable to use or respond to non-verbal communication (or are otherwise delayed in its use), such as pointing, gesturing and so forth, especially to indicate something of interest.
- People with ASD often have difficulties understanding abstract language/communication such as metaphors, sarcasm, colloquialisms and jokes.
- Repetitive behaviours, such as rocking, hand-flapping, finger movements and so forth, are common among people with ASD.
- People living with ASD are often highly sensitive to change, and they are “creatures of habit.”
- Most people with ASD have a range of sensory dysfunctions that vary widely (e.g., extreme sensitivities to noise, touch, smells, tastes, etc.) while many also exhibit a high pain threshold.
- Some children with ASD have exceptional abilities in music, visual and academic skills.
- In addition, up to 90% of children with ASD will have a co-existing medical and/or psycho-behavioural disorder, such as ADHD, anxiety, sleep disorders, feeding disorders, seizures, intellectual disability and gastro-intestinal disorders.
Early Intervention Supports Treatment for Children with ASD
Research suggests that early intervention is most impactful to the prognosis of ASD,3 and it can enhance the development of learning, communication and social skills for people living with the condition. Autism is typically diagnosed in early childhood, even as early as 18 to 24 months of age.
In many provinces, families experience long waiting times when seeking early diagnosis and/or intervention due to a “bottlenecking” of access to appropriate diagnostic centres – delays that can sometimes exceed two years.
Between 21% and 27% of military families do not have a family doctor, compared with 15% among the general population.4 Since many health services and treatments are accessed through family doctors, this discrepancy means that military families can have a harder time accessing services for children with special needs, including those with ASD. With each move, families who are moving toward the top of wait-lists for services find themselves back at the bottom.
Since many health services and treatments are accessed through family doctors, this discrepancy means that military families can have a harder time accessing services for children with special needs.
Exploring the Experiences of Military Families of Children with ASD
In a recent qualitative study, military families who have a child with ASD were interviewed to explore and describe their experiences navigating health care systems on behalf of their children.5
Many of these families reported that they had a hard time getting their child’s condition noticed, validated and medically diagnosed. Families generally found it difficult to get the assessment for ASD, and this delay in assessment and subsequent diagnosis meant that, for many, their access to intervention services was held up significantly.
One parent explained that their family experienced delays in accessing care for their son after moving because many of the programs available in their new community were for people living with autism who have a diagnosis. Since the family didn’t realize that they would need to have the diagnosis in hand when they sought care in their new neighbourhood, they went ahead and moved without having one, only to find that their son couldn’t access these programs as a result. Access to care for their child was delayed by months.
Difficulties accessing care can have an impact on family finances. Frustrated with wait-lists and the implications of delayed services for their child’s long-term development, many families opted instead to pay directly for private assessment services. One participant described making the decision to seek out private assessment and intervention because the wait-lists would exceed their posting tenure: “We paid privately… because the wait-list was too long. Once we had that diagnosis, [a community organization] put us on a wait-list for [Applied Behaviour Analysis] therapy. That wait-list is two years long. So we were never going to see the end of that wait-list either. So… we started paying privately for him.”
Frustrated with wait-lists and the implications of delayed services for their child’s long-term development, many families opted instead to pay directly for private assessment services.
At times, families waiting for care said they wound up moving again before their child’s name made it to the top of the local wait-list. For some families, service access was within sight, and then another posting forced them to move and start all over again. One participant shared that after waiting for some time for their child to get into a program, they finally received confirmation from their intervention team that the child would be able to start in September – which was of little help to them at that point, since they were going to be moving again in July.
With services varying widely from province to province (along with the corresponding eligibility and funding), some families reported consternation over losing services that they had previously had access to but were simply not available in their new location. One participant described this experience, “We realized the school [in the current province] didn’t offer the same things that they do in [the previous province]… there was nothing they could do…”
These variations also exist from region to region within the same province. For example, another participant described having to remove her child from a highly beneficial education program because they were moving, but then found they were unable to place him in a similar program in the new city because the program didn’t exist there (even though they were in the same province). Families in several other provinces described similar circumstances when moving interprovincially or intraprovincially.
Ongoing Pursuit of Health Care Affects Family Well-Being
While military families are highly resilient, difficulty accessing health care services for their children with ASD can have an impact on their own and their family’s well-being. Participants in the study commonly described frustration and confusion over the daunting tasks of sorting out how to get their children whatever services were possible. One participant described “bursting into tears” after finally getting to the top of a wait-list for intervention only to find the service did not meet expectations.
Some participants described having to draw on support from extended family to help care for their children. One participant said her parents retired and moved to the family’s current posting to assist because “they knew [our son] needed more help and we needed a break.” Others lamented the fact that extended family were too far away to really provide any assistance and were “just not able to be there.” Participants’ experiences with Military Family Resource Centres (MFRCs) were diverse, as the available services varied from base to base.
Parents often experienced strain on their relationships with their spouse or partner as their efforts to find caregiver supports and develop local networks can be complicated by training exercises, deployments and postings. As a result, hard choices are sometimes made related to whether or not a new posting, which comes with career opportunity, is feasible given the health care implications for the child with ASD.
Parents often experienced strain on their relationships with their spouse or partner as their efforts to find caregiver supports and develop local networks can be complicated by training exercises, deployments and postings.
Some participants described the Canadian Armed Forces (CAF) member making career decisions such as changing trades or requesting a specific posting for the benefit of the child, even though it could have an impact on their career trajectory and, by extension, the family as a whole. One participant said their family would consider living apart (i.e., imposed restriction) if it meant the child would receive the services needed, even though this would create a protracted separation that could have a significantly negative impact on the family as a whole.
In some military families, a civilian spouse may need to limit their involvement in the paid labour force to offset the caregiving requirements of the child. Such “trade-offs” are common in military families, with more than half (51%) of surveyed CAF spouses reporting that they have made some career sacrifices because of their partner’s military service, according to a 2009 study from the Director General Military Personnel Research and Analysis (DGMPRA). This limited workforce involvement can further constrain family finances that may be needed to pay for private services for their children. This can have a greater impact on dual-service families (families with two serving CAF members).
Military Families Express Desire for Navigation Support
Some military family members identified a few ways that could be considered to enhance the support for other military families who have children with ASD. Many expressed the desire to connect with other military families who are already at the new location to help map out options for how to access ASD-related services; some wanted this to be a formalized opportunity whereas others felt it would be important that it happen outside of official channels.
Many [families] expressed the desire to connect with other military families who are already at the new location to help map out options for how to access ASD-related services.
Opportunities to provide augmented and current information for families were also discussed, with some expressing a desire for a single point person who can help them navigate across school, community and health services. However, one participant indicated this type of formalized approach could result in parents receiving “filtered information” without any indication of how effective the services really are.
This qualitative study raised some important issues, but there is much left to learn. How might some of these opportunities be realized within existing formal and informal networks for incoming families? How could the disruptions and delays to health care access that military families report be reduced across provinces? What, if any, kinds of options might there be to offset the financial implications for parents when publicly funded services are absent or inaccessible? Are the differences for those who move within provinces similar to those who move across provinces? Exploring these questions through further research – with the insights and participation of families – will be key in supporting Canada’s diverse military families.
Dr. Heidi Cramm is the Interim Co-Scientific Director at the Canadian Institute for Military and Veteran Health Research (CIMVHR) and recipient of the 2016 Colonel Russell Mann Military Family Health Research Award.
Notes
- Heidi Cramm et al., “Making Military Families in Canada A Research Priority,” Journal of Military, Veteran and Family Health 1:2 (November 2015). Link: http://bit.ly/2zx46G1.
- Learn more with A Snapshot of Military and Veteran Families in Canada. Link: https://bit.ly/2fM3xmP.
- Geraldine Dawson, “Early Behavioral Intervention, Brain Plasticity, and the Prevention of Autism Spectrum Disorder,” Development and Psychopathology 20:03 (July 7, 2008). Link: https://bit.ly/2SWK2Lj.
- Nathan Battams, “A Snapshot of Military and Veteran Families in Canada,” Statistical Snapshots (November 2016). Link: https://bit.ly/2fM3xmP.
- Most of the families who participated in the study were married, and one-third of them had both parents serving in the Canadian Armed Forces (CAF). Most of the families represented serving members in the Regular Forces, primarily in the Army.
A Snapshot of Families and Food in Canada
Food is at the heart of family life. A biological necessity for our survival and well-being, food is also much more than that. What we choose to eat is often more than just a matter of personal preferences and whims; in many instances, what we eat reflects our cultural, community and family identities. Sometimes, our choices are made for us based on the availability and accessibility of food.
Regardless of the context, families adapt and react to ensure that dietary needs are being met. Some families have many opportunities to eat together, and these family meals provide a setting where family dynamics and relationships often “play out,” whether it’s in the delegation of cooking roles, discussing an upcoming family vacation or arguing over who has to do the dishes. Sometimes families – particularly those with busy schedules or high mobility – opt to eat meals “on the go.”
A Snapshot of Families and Food in Canada explores the evolving relationships between families and food in Canada, including research and statistics about family meals, eating patterns, nutrition, food security and more.
Highlights include:
- More than 6 in 10 Canadians (62%) surveyed in 2017 said they eat dinner as a family at least five times per week.
- More than one-quarter (26%) of Canadians surveyed in 2017 agree with the statement, “My work–life balance does not permit me to prepare and/or eat my meals at home.”
- The most recent data indicates that 12% of households across Canada (1.3 million) experienced food insecurity in 2014, home to 3.2 million people.
- More than half (52%) of Inuit living in Inuit Nunangat1 aged 25 and over lived in food-insecure households in 2012.
- In 2015, households across Canada spent an average $8,600 on food, an increase of 9.9% since 2010.
- 4 in 10 of those who said it’s become more difficult to afford groceries said they’ve been choosing less healthy options in the aisle to manage the rising prices.
- According to a 2017 study, more than three-quarters of Canadians aren’t meeting Canada Food Guide recommendations for fruit and vegetable consumption, with a resulting estimated economic burden to society of is $4.39 billion per year.
- More than 863,000 people across Canada accessed food banks in March 2016 alone (40% of whom lived in family households with children), 28% higher than in 2008.
- Research shows that the widespread malnutrition experienced by Indigenous children in Canada’s residential school system has had (and continues to have) a multi-generational impact on the health and well-being of their children and grandchildren, contributing to higher rates of chronic conditions.
This bilingual resource will be updated periodically as new data emerges. Sign up for our monthly e-newsletter to find out about updates, as well as other news about publications, projects and initiatives from the Vanier Institute.
Download A Snapshot of Families and Food in Canada from the Vanier Institute of the Family
This Statistical Snapshot publication is dedicated to David Northcott, CM, OM, retired Executive Director of Winnipeg Harvest Food Bank and a founder of both the Canadian Association of Food Banks and the Manitoba Association of Food Banks. David recently completed his second full term on the Vanier Institute Board of Directors, where his enthusiasm, dedication to family well-being and generous heart has had an impact on the entire Vanier Institute team.
Notes
- From Statistics Canada: “Inuit Nunangat is the homeland of Inuit of Canada. It includes the communities located in the four Inuit regions: Nunatsiavut (Northern coastal Labrador), Nunavik (Northern Quebec), the territory of Nunavut and the Inuvialuit region of the Northwest Territories. These regions collectively encompass the area traditionally occupied by Inuit in Canada.” Link: http://bit.ly/2gbzaqo.
Grandparent Health and Family Well-Being
Rachel Margolis, Ph.D.
Download this article in PDF format.
Canada’s 7.1 million grandparents and great-grandparents make unique, diverse and valuable contributions to families and society, serving as role models, nurturers, historians, sources of experiential knowledge and more. As with the general population, the grandparent population in Canada is aging rapidly, sparking some concern in the media and public discourse about the potential impact of this “grey tsunami.”
However, despite being older, data show that the health of grandparents has improved over the past 30 years. This trend can positively impact families, since healthy grandparents can have a higher capacity to contribute to family life and help younger generations manage family responsibilities such as child care and household finances.
Improving grandparent health enhances their capacity to contribute to family life and help younger generations manage family responsibilities.
Canada is aging, and so are its grandparents
The aging of the grandparent population mirrors broader population aging trends across the country. According to the most recent Census in 2016, 16.9% of Canada’s population are seniors, nearly double the share in 1981 (9.6%) and the highest proportion to date. This growth is expected to continue over the next several decades: projections show that nearly one-quarter (23%) of Canadians will be 65 or older by 2031. Furthermore, the oldest Canadians (aged 100 and over) are currently the fastest-growing age group: there were 8,200 centenarians in 2016 (up 41% since 2011), and projections from Statistics Canada show that this group is likely to reach nearly 40,000 by 2051.
In this context, it’s perhaps no surprise that the overall grandparent population is also aging. The share of grandparents who are seniors grew from 41% in 1985 to 53% in 2011, and the share of grandparents who are aged 80 and older has grown even faster, nearly doubling from 6.8% in 1985 to 13.5% in 2011.
Life expectancy increases fuel grandparent population aging
One of the underlying factors fuelling the aging of the grandparent population is the fact that Canadians are living longer. According to Statistics Canada, life expectancy at birth has continued to rise steadily, reaching 83.8 years for women and 79.6 years for men in 2011–2013. This represents an increase of about a decade over the past half-century, with women and men gaining 9.5 years and 11.2 years, respectively, since the years 1960–1962.
In addition, more people are reaching seniorhood than in the past because of mortality declines at ages below age 65. Data from Statistics Canada shows that the average share of female newborns who can expect to reach age 65 rose from 86% for those born in 1980–1982 to 92% for those born in 2011–2013, while this share increased from 75% to 87% for males during the same period.
People are also living longer as seniors, as reflected in ongoing increases in life expectancy at age 65 – a useful measure of the well-being of older populations since it excludes mortality for those who do not reach seniorhood. According to estimates from Statistics Canada, life expectancy at age 65 in 2011–2013 was 21.9 years for women and 19 years for men – up by 3 years and 4.4 years, respectively, from 1980 to 1982.
Delayed fertility contributes to the aging of the grandparent population since it increases the age of transitioning into grandparenthood.
Another contributing factor to the aging of grandparents is the fact that on average, women are having children at older ages than in the past – a fertility trend that increases the age of transitioning into grandparenthood. The average age of first-time mothers has risen steadily since 1970, from 23.7 to 28.8 years in 2013. The number of first-time mothers aged 40 and older has also grown, rising from 1,172 in 1993 to 3,648 in 2013 (+210%). As more women postpone childbearing until later in life, their transition to grandparenthood will also likely occur later. Today’s new grandparents are baby boomers, a generation in which many women delayed fertility for education and work experience. Their children are also having children later, and the fertility postponement of two generations together is influencing the pattern of later entry into grandparenthood.
Despite the aging of grandparents, grandparenthood accounts for a growing portion of many people’s lives. Even though people are becoming grandparents later, they are living longer as grandparents. The longer period of time spent in the grandparent role can extend opportunities for forming, nurturing and strengthening relationships with younger generations. According to my recent research, the average number of years that someone can expect to spent as a grandparent given today’s demography in Canada is 24.3 years for women and 18.9 years for men – that’s approximately two decades in which they can continue to play a major role in family life.
Despite being older, grandparents are healthier
In addition to living longer, data from the General Social Survey (GSS) suggest that grandparents in Canada today are far more likely to report living in good health than in the past. The proportion who rate their health as “good/very good/excellent” has increased from 70% in 1985 to 77% in 2011, while the share reporting “fair/poor” health has fallen from 31% to 23%. Overall, the odds of grandparents reporting that they are in good health are 44% higher in 2011 than in 1985.
A number of trends have contributed to health improvements among grandparents and older Canadians in general over the past half-century. There have been significant advances in public health that have facilitated disease prevention, detection and treatment. Among other factors, this has led to major reductions in deaths from circulatory system diseases (e.g. heart disease), which has been one of the biggest contributors to gains in life expectancy among men over the past half-century.
Another factor contributing to improvements in the health of grandparents in Canada is the rising educational attainment of this population. Research shows that education can improve health both in direct and indirect ways throughout life. Direct impacts can include enhancing one’s health literacy, knowledge, interactions with the health care system and patients’ ability and willingness to advocate for themselves when engaging with health care providers. Indirect impacts can include an increase in one’s resources (e.g. income) or occupational opportunities (e.g. being less likely to have a physically demanding and/or risky job, and more likely to have a job with health benefits).
Education has been associated with greater health, which is significant because the share of grandparents who have completed post-secondary education has more than tripled over the past three decades.
These are important factors to consider in the Canadian context, since the share of grandparents who have completed post-secondary education has more than tripled over the past three decades, from 13% in 1985 to nearly 40% by 2011.
Healthy grandparents can facilitate family well-being
Grandparent health can have a significant impact on families. When a grandparent (or multiple grandparents) is living in poor health, families are often the first to provide, manage or pay for care that supports their well-being. This is particularly true for senior grandparents receiving care at home; the Health Council of Canada estimates that families provide between 70% and 75% of all home care received by seniors in Canada.
Data from the 2012 GSS show that nearly 3 in 10 Canadians (28%) reported providing caregiving to a family member in the past year, and aging-related needs were the most commonly cited reason for care (reported by 28% of caregivers). Grandparents accounted for 13% of all Canadians who received care, and they were also the most frequent recipients of young caregivers’ (aged 15 to 29) assistance, 4 in 10 of whom cited a grandparent as the primary recipient.
While 95% of caregivers say they’re effectively coping with their caregiving responsibilities, research has found that in some contexts, it can have a negative impact on their well-being, career development and family finances. This can be particularly true for the three-quarters of caregivers who are also in the paid labour force, accounting for more than one-third of all working Canadians.
On the other hand, when grandparents are living in good health, families can benefit in a variety of ways. In addition to the fact that it means they are less likely to require caregiving assistance, they are also more likely to be able to make positive contributions to family life, such as providing child care and contributing to family finances.
Grandparents provide child care to younger generations
Many grandparents play an important role in caring for their grandchildren, which can help parents in the “middle generation” manage their child care and paid work responsibilities. A number of economic, social and environmental trends have converged in recent decades that have increased the significant contributions they make to families with regard to child care.
Many grandparents play an important role in caring for their grandchildren, which can help parents in the “middle generation” manage their child care and paid work responsibilities.
Over the past four decades, the share of dual-earner couples in Canada has increased; in 1976, 36% of couples with children included two earners, a rate that nearly doubled to 69% by 2014. In more than half of these couples (51%), both parents worked full-time, which means they were more likely to rely on non-parental care for their children. This is supported by data from the 2011 GSS: while nearly half (46%) of all parents reported relying on some type of child care for their children aged 14 years and younger in the past year, the rate was higher (71%) for dual-earner parents with children aged 0 to 4 and children aged 5 to 14 (49%).
The evolution in family structure and composition across generations has also contributed to more families relying on non-parental care for their children. The share of lone-parent families has increased significantly over the past 50 years, rising from 8.4% of all families in 1961 to approximately 16% in 2016. Data from the 2011 GSS show that nearly 6 in 10 lone parents of children aged 4 and under (58%) report that they rely on non-parental care.
Sometimes grandparents are solely responsible for raising their grandchildren when no middle (i.e. parent) generation is present. The 2011 GSS counted 51,000 of these “skip-generation families” in Canada, which was home to 12% of all grandparents who live with their grandchildren. Some of those who live with their children are more likely than others to live in skip-generation homes, such as people reporting a First Nations (28%), Métis (28%) or Inuit (18%) identity (compared with 11% among the non-Indigenous population).
Lastly, many parents may rely on grandparents for help with child care if they can’t find quality, regulated child care spaces in their communities. In 2014, the availability in regulated, centre-based child care spaces was only sufficient for one-quarter (24%) of children aged 5 and under across Canada. While this is a significant increase from 12% in 1992, it still leaves more than 3 in 4 children in this age group without an available regulated child care space. The availability of child care (or a lack thereof) is significant, since it can affect whether or not parents in coupled families can both participate in the paid labour market.
The cost of child care can also lead parents to turn to grandparents for child care assistance. This is particularly true for families living in urban centres. One 2015 study on the cost of child care in Canadian cities, which used administrative fee data and randomized phone surveys conducted with child care centres and homes, found that the highest rates in Canada were in Toronto, where estimates showed median unsubsidized rates of $1,736 per month for full-day infant care (under 18 months of age) and $1,325 for toddlers (aged 1½ to 3).
Grandparent involvement can enhance child well-being
Regardless of the reason grandparents spend time with their grandchildren, their involvement in family life can benefit the well-being of children. Studies have shown that grandparent involvement in family life is significantly associated with child well-being – in particular, it has been associated with greater prosocial behaviours and school involvement. The benefits aren’t limited to children, either, as other research has shown that close relationships between grandparents and grandchildren can have a positive impact on mental health for both. Among First Nations families, grandparents have also been found to play an important role in supporting cultural health and healing among younger generations.
Research shows that grandparent involvement in family life is significantly associated with child well-being, including greater prosocial behaviours and school involvement.
The broader context of improving grandparent health is good news for many families, since their better health can make it easier to participate in activities with children and grandchildren, and research shows that these interactions with younger kin can be more rewarding in this context.
Many grandparents play an important role in family finances
Improvements in grandparent health can also enhance their capacity to engage in paid work, which can improve their own finances and facilitate contributions to younger generations.
Improvements in grandparent health also enhance their capacity to engage in paid work, which can improve their own finances and facilitate contributions to younger generations.
While there isn’t much recent data on the employment patterns of grandparents in Canada per se, rising rates of working seniors have been well documented over the past several decades. Between 1997 and 2003, the paid labour force participation rate for seniors ranged between 6% and 7%, but this has steadily increased to around 14% in the first half of 2017 (and an even higher rate of 27% for those aged 65 to 69). Since approximately 8 in 10 seniors in Canada are grandparents, it’s clear that a growing number of grandparents are working today.
The potential for grandparents to contribute to family finances through paid work can be particularly important for the 8% who live in multi-generational households. According to data from the 2016 Census, this is the fastest-growing household type, having grown in number by nearly 38% between 2011 and 2016 to reach 403,810 homes. Similar to patterns found among skip-generation families, this living arrangement is more common among Indigenous and immigrant families, which both represent a growing share of families in Canada.
Skip-generation living arrangements are more common among Indigenous and immigrant families, which both represent a growing share of families in Canada.
Data from the 2011 GSS showed that among the 584,000 grandparents living in these types of homes, more than half (50.3%) reported that they have financial responsibilities in the household. Some were more likely than others to contribute to family finances: rates were significantly higher for those living in skip-generation households (80%) and multi-generational households with a lone-parent middle generation (75%).
Opportunities are growing for grandparent–family relationships
While the aging of the general and grandparent population in Canada presents certain societal challenges, notably with regard to community care, housing, transportation and income security, their rising life expectancy and improving health present growing opportunities for individuals and families. Many grandparents already help younger generations with fulfilling family responsibilities, such as child care and managing family finances, and this will continue in the years ahead – a positive side of the story that is often lost in narratives about the “grey tsunami.”
As the health of grandparents has improved over the years, many have been able to enjoy a greater quantity and quality of relationships with younger family members. As families adapt and react to their evolving social, economic and cultural contexts, they will continue to play an important – and likely growing – role in family life for generations to come.
Rachel Margolis, Ph.D., is an Associate Professor in the Department of Sociology at the University of Western Ontario.
All references and source information can be found in the PDF version of this article.
Published on September 5, 2017
Facts and Stats: Families and Active Leisure in Canada (2017 Update)
Whether it’s swimming at the beach in the summer, tobogganing in the winter or playing organized sports throughout the year, many families enjoy being physically active in their leisure time, and this exercise can have a positive impact on our individual and family well-being. However, there is growing concern that many people aren’t meeting the recommended guidelines for physical activity, as busy schedules and “screen time” can interfere with our best efforts to keep moving.
Learn about how Canadians of all ages are keeping fit and having fun with our updated fact sheet on families and active leisure in Canada!
Download Facts and Stats: Families and Active Leisure in Canada from the Vanier Institute of the Family.
Published on July 25, 2017
In Context: Understanding Maternity Care in Canada
If it takes a village to raise a child, it certainly takes one to bring a child into this world. New and expectant mothers receive care from many people throughout the perinatal period, and the networks and relationships that support them can play a major role in ensuring the health and well-being of new mothers and their newborns.
Childbirth is a milestone, an exciting time when the family grows and a new generation begins. It’s also a period of significant child development – a time of great vulnerability but also of great opportunity to benefit from healthy nurturing.
The experience of pregnancy, childbirth and postnatal care continues to evolve through the generations. Rates of maternal mortality (women dying as a result of pregnancy and childbirth), maternal morbidity (women developing complications as a result of childbirth) and infant mortality all saw significant declines throughout the 20th century following medical advances and improvements in maternal care, nutrition and general living standards.
Maternal and Infant Mortality in Canada
Maternal mortality dropped from 508 deaths per 100,000 live births in 1931 to 7 per 100,000 in 2015.
Infant mortality rates fell from an average of 76 deaths per 1,000 live births in 1931–1935 to 4.9 per 1,000 in 2013.
In the 1800s to the mid-1900s, maternity care in Canada typically took place in the local community and birth occurred in the home, with families and midwives routinely providing care to new and expectant mothers. However, with the development of medicare throughout the 20th century, births and maternity care gradually moved into hospitals and medical clinics, with care being delivered primarily by medical professionals such as doctors and obstetricians – a trend sometimes referred to as the “medicalization of childbirth.”
By the early 1980s, the vast majority of births occurred in regional hospitals, where family physicians or obstetricians were present and assisted by obstetrical nurses. Partners and other family members became largely left out of the childbirth process, often relegated to waiting rooms. Following birth, babies were placed in nurseries, separated from their mothers – a situation that was sometimes traumatic for mothers and their newborns.
Hospitals eventually started allowing the rooming in of mother and baby to facilitate mother–infant attachment and support breastfeeding for the health and well-being of both. During the rooming-in period, nurses would provide new mothers with information for the recovery period, such as instruction about breastfeeding and postnatal care. Throughout this transition in postnatal care practices, the length of time women spent in hospital after having a baby decreased significantly, from an average of nearly five days in 1984–1985 to 1–2 days after vaginal delivery today.
Today, partners are more involved in the birthing process and the perinatal period generally than in the past. Most are present for births, taking on a greater role in these first moments of their children’s lives and in the child rearing in the years that follow. It is more common for couples today to conceptualize childbirth as a shared experience, and many people use language that reflects this trend (“We’re expecting,” etc.).
What is maternity care?
Maternity/perinatal care (hereafter referred to as maternity care) is an umbrella term encompassing a continuum of care provided to the mother and child before, during and after birth. This includes prenatal/antenatal care (care during pregnancy), intranatal care (care during labour and delivery) and postnatal/postpartum care (care for the mother and newborn following birth). Since both mothers and infants undergo major changes throughout the perinatal period, maternity care entails a diverse range of health monitoring and care.
Prenatal/antenatal care (hereafter referred to as prenatal care) monitors and supports the health and well-being of mothers and the developing fetus prior to birth. Fetal health is monitored through screening and diagnostics, such as ultrasounds and blood tests. Health providers also closely track the mother’s health during this period; expectant mothers are provided with information about pregnancy, fetal development, physical comfort, testing, planning for delivery and preparing for parenthood.
Most women (87%) say they were supported by a partner, family or friends throughout the prenatal period.
According to the 2009 Canadian Maternity Experiences Survey, most women (87%) say they were supported by a partner, family or friends throughout the prenatal period. This support, as well as the care provided by health practitioners, can be particularly important during this time when many (57%) women report most days as being stressful. During pregnancy, maternal stress can have an impact on the well-being of the baby, leading to premature birth and/or low birth weight.
Nearly all expectant mothers (95%) report that they started prenatal care in their first trimester. Certain groups were more likely than others to report that they did not start prenatal care in the first trimester, however, such as women aged 15–19 years, those with less than high school education or those who live in low-income households. One of the main reasons cited for not starting care early in the pregnancy was lack of access to a doctor or health care provider.
Intranatal/intrapartum care (hereafter referred to as intranatal care) refers to the care and assistance provided to mothers during labour and childbirth. This involves facilitating the delivery itself in a safe and hygienic manner as well as monitoring the health of mother and child throughout the delivery process. This care is most often provided in hospitals, with mothers receiving care from a variety of health practitioners including obstetricians/gynecologists (reported as the main health care provider during labour and birth by 70% of surveyed mothers), family doctors (15%), nurses or nurse practitioners (5%) or midwives (4%).
Whether provided by a spouse, partner, friend, family member, midwife or doula (or some combination thereof), emotional support during this time is important. Research shows that women who receive continuous social support are more likely to have a shorter labour (i.e. fewer hours) and a vaginal birth, are more likely to report feeling happy with their labour and birth experience and are less likely to use pain medication.
Research shows that women who receive continuous social support are more likely to have a shorter labour and a vaginal birth, and are more likely to report feeling happy with their labour and birth experience.
Postnatal/postpartum care (hereafter referred to as postnatal care) supports mothers and newborns following childbirth, and involves health monitoring and routine assessments to identify any deviation from expected recovery following birth, and to intervene, if necessary.
The postnatal period accounts for the first six weeks of a child’s life – a “critical phase” in which examinations and care from health practitioners play an important role in ensuring the well-being of the mother and child, according to the World Health Organization (WHO).
In their 2013 postnatal care guidelines, WHO outlines best practices including postnatal care in the first 24 hours to all mothers and babies (regardless of where the birth occurs), ensuring that healthy women and their newborns stay at a health facility at least 24 hours and are not discharged early, and have at least four postnatal checkups in the first 6 weeks following childbirth.
According to the Maternity Experiences Survey, more than 7 in 10 women (73%) rated their health as “excellent” or “very good” by 5 to 14 months postpartum. However, more than 4 in 10 women in Canada (43%) said they experienced a “great deal” of problems with at least one postpartum health issue during the first three months following childbirth, such as breast pain (16% of women), pain in the vaginal area or in the area of the caesarean incision (15%) and back pain (12%).
Postnatal support can be important in mitigating postpartum depression, which is reported by 10%–15% of mothers in developed countries. Research has shown that maternal stress during pregnancy, the availability of social support and a prior diagnosis of depression are all significantly associated with developing postpartum depression. Studies have also shown that emotional support from partners and other family members throughout the perinatal period can reduce the likelihood for postpartum depression and emotional distress for mothers and newborns.
Postnatal care services vary across regions and communities in Canada. These can include informational supports, home visits from a public health nurse or a lay home visitor, or telephone-based support from a public health nurse or midwife.
Privately delivered postnatal services have become more prevalent over the past several decades, with postpartum doulas advertising high-intensity supports such as newborn care, breast- and bottle-feeding support, child-minding services, meal preparation, household chores and more. However, these private services often involve out-of-pocket costs that can limit accessibility for some families.
Who provides maternity care?
In addition to the care and support provided by family members and friends, modern maternity care is delivered by a range of health practitioners including family physicians, obstetricians/gynecologists, nurses, nurse practitioners, midwives and birth doulas – all of whom make unique contributions in the continuum of care.
Family physicians provide care to most new mothers throughout the perinatal period and can be involved in all stages of maternity and infant care, though not all provide the full range of care. Fewer physicians across Canada are providing maternity care than in previous decades: the share of family physicians in Canada delivering babies declined from 20% in 1997 to 10.5% in 2010. Today, a growing number of care tasks and responsibilities are being delivered by other medical practitioners, such as obstetricians and midwives.
Most family physicians who report being involved in maternity and newborn care provide “shared care,” offering prenatal care to a certain point (often between 24 and 32 weeks), after which they transfer care to another provider (e.g. obstetricians, midwives or another family physician who delivers babies). Some attend deliveries, but rates vary widely between provinces and the availability of other health providers.
Obstetricians and gynecologists (OB/GYNs) are providing a growing amount of intranatal care in Canada – though not all do so, and rates vary across the provinces. With specialized knowledge and expertise in pregnancy, childbirth and female sexual and reproductive health care (including surgical training, such as caesarian sections), many also serve as consultants to other physicians and are involved in high-risk pregnancies.
Nurses constitute the largest group of maternity care providers in Canada. They can be involved throughout the entire perinatal period, providing a range of care services including childbirth education, pre-birth home care services to women in high-risk situations, assistance during childbirth and sometimes follow-up care to new mothers. Following childbirth, nurses often provide information to new mothers while preparing them for discharge, educating them about topics such as breastfeeding, bathing, jaundice, safe sleep, postpartum mental health, nutrition and more.
Nurse practitioners (NPs) are registered nurses who play a wide variety of roles in health care. They sometimes serve as primary care providers for low-risk pregnancies, performing a variety of tasks such as physical examinations, screening and diagnostic tests, and postnatal care. When providing or facilitating maternity care, NPs often work in interdisciplinary teams with other health professionals such as physicians and midwives. In hospital settings, they also work in labour and delivery units, postpartum units, neonatal intensive care units and outpatient clinics. Due to the breadth of their training and expertise, NPs play important roles in rural and remote communities, where many provide a full range of health care services.
Due to the breadth of their training and expertise, nurse practitioners play important roles in rural and remote communities, where many provide a full range of health care services.
Midwives provide primary care to expectant and new mothers throughout the entire perinatal period, and are playing a growing role in modern maternity care in Canada. They provide a range of care services, including ordering and receiving tests, accompanying women at home or in birthing centres, admitting women for hospital births, as well as assisting with breastfeeding, the early days of parenting and monitoring postpartum healing. Midwives work collaboratively, consulting with, or referring to, other medical professionals when appropriate.
The role of midwives has evolved over the past several decades, with a growing number assisting in all settings where care may be needed – at home, in the community and in hospitals, clinics or health units. There has been increasing emphasis on specialization and training, as midwives have become recognized by and incorporated into most (but not all) provincial/territorial health care systems across the country.
Doulas provide non-clinical/medical support, working with new mothers and their families as well as health care practitioners such as physicians, midwives and nurses. Doulas are not regulated; they focus largely on emotional and informational support, and they do not provide direct health care or deliver babies.
There are different types of doulas for different stages in the childbirth process. Antepartum doulas provide emotional, physical and informational support during the prenatal period. This can include informing new mothers and their families about support groups, techniques for enhancing physical comfort and helping with home care tasks such as errands and meal preparation. Birth doulas support new mothers and their partners during labour and delivery, including emotional and informational assistance and supporting physical comfort. Postpartum doulas support new mothers after the baby is born, providing information about topics such as infant feeding and soothing techniques, and sometimes helping with light housework and childcare.
Perinatologists provide care in the event of high-risk pregnancies (e.g. pregnancy in the context of chronic maternal health conditions, multiple births or genetic diagnoses). They are trained as OB/GYNs and then receive specialized education to facilitate complicated pregnancies. OB/GYNs refer patients to perinatologists when needed, but continue to work collaboratively to support maternal health.
Unique experiences: childbirth in rural and remote areas in Canada
Maternity care in rural and remote areas (including Canada’s northern regions) faces unique challenges due to distances from medical facilities and specialized equipment, less peer support for care providers, as well as a limited number of physicians available for on-call services, and fewer caesarean section and anaesthesia capabilities/services compared with urban centres.
Rural maternity care is most often provided by teams of family physicians, nurses and midwives – in fact, in some communities, they’re the only health practitioners providing maternity care. Rural family physicians are far more likely to provide obstetrical care than their urban counterparts, though over the past several decades, many rural communities have seen a reduction in the number of family physicians providing maternity care and closures of maternity wards.
Due to the limited availability of maternity care providers and services in rural and remote regions, many expectant mothers travel to urban centres to give birth. According to a 2013 report from the Canadian Institute for Health Information, more than two-thirds of rural women in Canada (67%) report that they gave birth in urban hospitals, 17% of whom travelled more than two hours to deliver their babies. Rates are far higher in the North: two-thirds of surveyed mothers in Nunavut and half of those in the Northwest Territories report that they gave birth away from their home community.
Two-thirds of surveyed mothers in Nunavut and half of those in the Northwest Territories report that they gave birth away from their home community.
This has an impact on the well-being of many Indigenous women living in northern regions, many of whom have had to fly to hospitals far from their homes, land, languages and communities to receive maternity care at tertiary or secondary care hospitals (see Indigenous Midwifery in Canada textbox). When surveyed, the majority of mothers reported that leaving home to have their babies was a stressful experience and that it had a negative impact on their families. In April 2016, the federal government announced that it would provide financial compensation to allow someone to travel with Indigenous women who need to leave their communities to give birth.
The number of community hospitals offering obstetrical care in northern regions has fallen since the 1980s. However, a number of birthing centres have opened to fill this care gap, such as in Puvirnituq (Nunavik), Rankin Inlet (Nunavut) and in Inukjuak (Quebec). These facilities have helped women with low-risk pregnancies remain in their communities; however, those with complications or requiring a caesarian birth often still have to travel to give birth.
Unique experiences: new and expectant mothers new to Canada
Canada is home to many immigrant families, which have represented a growing share of the total population. In 1961, 16% of people in Canada reported that they were born outside the country – a rate that increased to 21% by 2011.
Immigration has an impact on the maternity experiences, such as when women decide to have children. Research shows that immigrants have relatively fewer births in the two-year period before migration, which is often followed by a “rebound” in fertility afterward. According to researchers Goldstein and Goldstein, “Fertility preferences of movers may more closely resemble those of the destination country than those of the source country even before they arrive.”
Studies have explored a number of reasons why fertility can be affected by the immigration experience, including temporary separation of spouses during the migration process, a conscious decision to delay childbearing until access to supports such as child allowances is ensured and economic disruption during migration and in the early period (while parents are securing paid employment).
Recent immigrants are significantly more likely than their Canadian-born counterparts to live in multi-generational households (those with three or more generations living under one roof); 21% of immigrants aged 45 and older who arrived in Canada between 2006 and 2011 reported that they live in shared homes, compared with 3% of the Canadian-born population. As such, new and expectant mothers in multi-generational homes may benefit from having more family members nearby to provide care and support.
With regard to accessing maternity care services, research has shown that many immigrant women generally have the opportunity to receive the necessary maternity care services, but rates of satisfaction with maternity care vary greatly across Canada. Some report having faced barriers to accessing and utilizing maternity care services, including (but not limited to) a lack of information about or awareness of the services (sometimes the result of language barriers), insufficient support to access the services (i.e. navigation of the health care system) and discordant expectations between immigrant women and service providers. In some areas, doulas provide valuable emotional, informational and navigation support to immigrant women during the perinatal period.
Social support (e.g. from family, friends and community members) has been identified by immigrant parents as a key factor in accessing maternity care. This circle of support can play an important role in connecting new and expectant mothers from outside Canada with maternity care, and can work with health care and service providers to ensure these women receive “culturally congruent and culturally safe” maternity care.
Maternity care: supporting Canada’s growing families
Pregnancy and childbirth are major life events, not only for new mothers, but also for their families, friends and communities. While there have been many changes in family experiences over the generations regarding pregnancy, childbirth and the postnatal period, there have also been some constant threads: the value and importance of quality care, the diversity of experiences across Canada, and the joy and excitement that can accompany this memorable and life-changing milestone.
Download this article in PDF format.
This content was reviewed by Dr. Marilyn Trenholme Counsell, OC, MA, MD, retired family physician and former Lieutenant Governor (New Brunswick), former Minister of Family (N.B.) and Senator (N.B.).
All references and source information can be found in the PDF version of this article.
Published May 11, 2017
Lived Experience: Understanding Families Affected by Incarceration
Farhat Rehman
Incarceration has an impact on thousands of families across Canada. When a person is sentenced to time in prison, their families are often profoundly affected; they are separated from a son, daughter, sibling, parent or other relative. Feelings of stigma, guilt and shame are common, and can be compounded when the sentenced family member is also living with a mental health condition – a reality for many incarcerated individuals and their families.
My family life has been profoundly affected by incarceration ever since my son was sentenced in 2001. When the chasm of the prison system had swallowed him up, the world appeared dark with no hope of seeing daylight. Our lives took a drastic turn on that ominous day. Our family’s lives and relationships were forever changed.
As a mother, I couldn’t help but wonder over and over again why my son had committed such a serious criminal act. Why did his mind work this way? What could have been done to prevent this catastrophe? Why, after years of treatment in the mental health system, had he still fallen through the cracks? What could I have done differently that would have prevented this crime from taking place and tearing apart two families? Since then, there have been daily reminders as I speak to him and visit him in prison. For us, his family, the impact of my son’s action have sunk in gradually over time. The nightmare of prison has played havoc with his mental health conditions with all the ups and downs of a roller coaster, and it’s become a constant source of worry for our family.
The nightmare of prison has played havoc with his mental health conditions with all the ups and downs of a roller coaster, and it’s become a constant source of worry for our family.
Incarceration affects family relationships, family traditions and family futures
As we have learned, in-person visits can be traumatic for the visitor. When visiting someone in prison, you have to first pass through layers of security such as the ion scanner (a drug-scanning device known for detecting false positives). Otherwise, you risk being turned away, which can seriously impact the inmate’s prison life.
There is no occasion that is celebrated as a family where I don’t feel my son’s absence. The festivities, the good food and laughter lack the genuine happiness that can come from family gatherings. This is never really talked about openly.
Family members will occasionally ask about my son and he may receive birthday cards from family and friends, but there is a kind of hesitation to discuss such a sad subject and ruin a festive atmosphere. The fact a family member has not been seen among you for almost 16 years registers low on the Richter scale of family life.
These days, as I contemplate the possibilities of the future, I wonder if this will be the time that my son will be able to start to turn his life around. Will he convince the authorities that he is deeply remorseful and resolved to never offend again? Will he be seen as worthy of being allowed to be paroled out of prison and into the community, where he can start the long process of healing and repairing the ravages of a lengthy period of incarceration? Will he be able to reintegrate himself into our family, one that misses him terribly but has adapted to life in his absence?
The love and light of support gets families through
While I contemplate these questions daily, I am grateful for the support of those around me. When my son – and my family – first began our journey with the justice system, I felt like I was travelling down an uncharted road. Despite being well connected to community, there was no real support I could turn to where others would understand what it was like to have a son in prison.
Despite being well connected to community, there was no real support I could turn to where others would understand what it was like to have a son in prison.
In November 2010, a community activist and expert connected to the Church Council on Justice and Corrections and a crisis worker at the John Howard Society (JHS) introduced me to another mother with a son in prison. We all met for the first time at JHS in December 2010 – three mothers coming together with common experiences and goals.
From this shared experience, Mothers Offering Mutual Support (MOMS), a support group for women, was born. The first formal MOMS meeting occurred on December 15, 2010. Our meetings take place at the local JHS building, during the first Thursday of the month. JHS has generously donated this space to us so we can meet in a location with privacy.
We now total more than 45 members, all of whom feel immensely grateful to be able to come together and climb out of the black hole we fell into when our children were convicted of an offence resulting in their incarceration. Now we come together to support each other and find ways to help them in a meaningful and constructive way. Mothers whose sons have completed their sentence or are on parole continue to support and guide the new members who join the group.
A loving family on the outside can play an important role in advocating, financially supporting and providing loving contact to offset the indelible ravages of incarceration. Through MOMs, we are able to support each other as we support our incarcerated children.
A loving family on the outside can play an important role in advocating, financially supporting and providing loving contact to offset the indelible ravages of incarceration.
The harsh realities of incarceration are with us, but together we encourage each other to take one day at a time. We have been working to ensure the justice system facilitates rehabilitation and education, with a focus on physical and mental well-being and supporting our sons or daughters while they serve their sentences and plan for their futures. This has provided us with opportunities to engage in dialogue with government and community leaders about human rights. Policies and programs benefit from understanding our lived experiences and our perspective as mothers. We have been encouraged by increased public awareness of these issues.
As you can imagine, for some moms and family members, issues of stigma and safety keep us fearful of speaking out publicly, even though we are worried sick and lose sleep thinking about the condition of our children. We do not want to add to our shame and worry by being on the receiving end of insensitive or negative comments.
As mothers affected by incarceration, we meet regularly to share our experiences and our shock, pain and heartbreak. Working together gives us energy to focus on strategies to equip ourselves with knowledge and best practices to keep ourselves and our loved ones hopeful and healthy. We are determined to achieve humane and just treatment for our loved ones in prison as we work together to strengthen the ties that bind us in our struggle as families affected by incarceration.
Farhat Rehman is co-founder of Mothers Offering Mutual Support (MOMS), a support group for women with incarcerated family members.
Download this article in PDF format.
Published on March 14, 2017
Supporting the Health of Mothers and Their Babies in the Context of Incarceration
Dr. Ruth Elwood Martin and Brenda Tole
When a friend told Ruth Elwood Martin that there was a need for a part-time family physician to work in a women’s correctional centre, her immediate thought was that there was no way she could work in a prison clinic. She perceived that it was the lowest kind of medical job, only for those doctors who were unable to find any other type of work.
Ruth is not sure what drew her to start practising medicine in a prison, but she did. On that first day in 1994, she felt like she was visiting another planet, passing through those gates, experiencing another world and learning from the people inside it. Ruth saw more pathology and more tragic medical diagnoses than she had seen in a year in her regular family practice in Vancouver’s West Side.
In the clinic, women told her about traumatic events they endured as children, young teenagers and women. Ruth would put down her pen, bearing witness to their lives, and listen to medical and social histories she could not imagine enduring. That first day in her new position changed Ruth’s life forever and she knew that prison health would become her calling. Ruth has often reflected that if she had been dealt the same childhood cards as the women she met, she might be sitting in their chairs.
In 2003, Brenda Tole was assigned to oversee the remodelling of an older facility that had housed provincially incarcerated men and to open it as the “Alouette Correctional Centre for Women” (ACCW), a medium-security facility to house provincially sentenced women. If you are a parent with school-aged children, you will have noticed how the school principal greatly influences the overall ethos of a school. In a similar manner, the warden of a prison influences the ethos of the institution, which in turn influences the overall health of the inmates.
From the day it opened in 2004, Brenda shaped the tone and ethos of ACCW. She maintained that if you expect both staff and incarcerated individuals to treat each other with respect, they will rise to meet those expectations, at least most of the time. That’s how she planned and that’s how she ran ACCW, not on the basis that 1% of the population may breach those expectations.
Brenda knew that the more she gave people opportunities, the more they valued the opportunities and responded positively. The more she gave responsibility to the women for doing things themselves, and the more she talked with the staff about her plans, the better the situation would be for everyone.
During a meeting of key health care players planning for health care delivery at the new ACCW, Brenda met Sarah Payne, the director of Fir Square at BC Women’s Hospital, a maternity unit for substance-using mothers. Babies who remained with moms at Fir Square had positive health outcomes compared with the health of babies that were taken away from their moms at birth.1 Sarah asked Brenda to consider the possibility that babies born to incarcerated mothers who came to the BC Women’s Hospital for their delivery might return with their mothers to ACCW, in order to foster breastfeeding, attachment and nurturing.
Separation through incarceration negatively affects the health of new mothers and their infants
With peer-reviewed academic literature growing on the subject, Brenda had good reason to consider this proposal. Evidence shows that one of the most compelling motivators for incarcerated women is pregnancy and their children. International correctional practices that promote contact between women and their children have shown benefits for both. Positive results have been seen in visits, email, tapes, telephone calls and letters. Children of incarcerated women are negatively impacted if the contact with their mother is limited or absent. Although it is accepted around the world that nursing infants and/or small children benefit from remaining with their incarcerated mothers, this was rarely seen in Canada at that time.
Many incarcerated women have dependent children. Worldwide, an estimated 6% of incarcerated women are pregnant while serving prison time.2 An estimated 20,000 children each year are affected by the incarceration of their mothers in Canada,3 where women tend to be held in correctional centres that are large distances from their children and families due to the limited number of correctional facilities for women across the country.
The provision of mother–child units to women in prison who have given birth to their infants while incarcerated is considered normal practice in most countries in the world. Published reports of such units exist for 22 countries, including England, Wales, Australia, Brazil, Denmark, Finland, Germany, Greece, Italy, the Netherlands, New Zealand, Russia, Spain, Sweden, Switzerland, some US states, Kyrgyzstan, Ghana, Egypt, Mexico, India and Chile.4, 5, 6
One of the reasons for keeping incarcerated mothers with their newborn babies is that it facilitates breastfeeding, which the World Health Organization reports has health benefits for the infant and new mother.7 According to international health experts, babies should be exclusively breastfed until they are six months old if possible, and then continue to be breastfed on demand until they are two years of age. Babies who are not breastfed may be at increased risk for diabetes, allergies and gastrointestinal and respiratory infections.8
In addition to the well-known health and nutritional benefits, some research has shown that breastfeeding can contribute to psychosocial development9 – the associated physical contact, eye contact and the quality of feeding promote mother–child attachment. However, establishing and maintaining breastfeeding on demand is not possible unless mothers and babies can be housed together with 24-hour contact.
Typically, mothers who return to prison without their babies after giving birth are prescribed milk-binding pills and are often prescribed antidepressants. In this situation, many mothers experience profound grief and debilitating guilt, despair and hopelessness. Many resort to substance use as a coping strategy.
Mother–child unit developed to support well-being of incarcerated mothers and their babies
In 2005, Brenda asked Ruth, “As the prison physician, what is your opinion about the idea of incarcerated women who deliver babies in hospital being able to return here with their babies?” Ruth felt it was the most sensible idea she had heard in years, and she then expanded her prison medical practice to perform new roles, such as newborn examinations, breastfeeding coaching and addressing medical questions about newborns.
Through collaboration and partnership with several other ministries and community agencies, a mother–child unit was developed at ACCW based on the best interests of the child. With the support of Corrections Branch Headquarters, the ACCW health care team, correctional staff (both managers and frontline staff) and other provincial ministry personnel, it was decided ACCW could facilitate the return of mothers and babies to ACCW when recommended by BC Women’s Hospital and agreed to by the Ministry of Children and Family Development (MCFD), who had final authority over the placement of the child.
The decisions to place the mother and child together at the correctional facility were made by an interdisciplinary team consisting of the key staff from BC Women’s Hospital, ACCW health care, ACCW administration and the MCFD. If the mother was Indigenous, the pertinent Indigenous communities were consulted, when applicable. The mother and her family were included in all stages of this process. The support and services that Fir Square offered the mother before and after the birth fostered the mother’s confidence in parenting and in participating in the planning of her future and that of her baby. All checks and balances were put in place to ensure that ACCW was a safe and positive environment for the mothers and babies, with the cooperation of the mothers, other incarcerated women and correctional staff.
Incarcerated women who gave birth and who were deemed by MCFD able and willing to provide appropriate parental care were allowed to keep their infants in their care while in prison. During the initiative’s duration (2005–2007), 13 babies were born to incarcerated mothers, nine of whom lived in prison with their mothers and stayed there until their mother’s release. Eight babies were breastfed for the duration of their mother’s prison stay. Fifteen months was the longest stay of any infant in prison. The babies’ health and development was monitored by the community public health nurses, ACCW health care providers and MCFD social workers.
Release planning for the majority of the mothers and babies included placement at a residential supportive residence for women with substance use histories of the Fraser Health Authority, which took mothers and their young infants. The residential placement staff aimed to facilitate the transition of these women into the community.
Being involved in the initiative with BC Women’s Hospital had a profound positive effect on the women directly involved, the correctional staff and other incarcerated women, and the ministries and community agencies who partnered with ACCW.
Mother–child unit facilitates maternal involvement
Initially, other agencies and ministries were surprised and cautious regarding the proposal of the newborn babies returning to the facility with their mothers. The team at ACCW and BC Women’s Hospital took the time and facilitated many discussions and held meetings for all stakeholders to contribute to the program’s success.
Initially, the rights of the infant to be with the mother for attachment, bonding and breastfeeding was overshadowed for some by the feeling that this “privilege” should not be afforded to incarcerated mothers. As the initiative continued, the attitudes of many began to shift from cautious and guarded to comfortable and supportive. Community agencies were willing to provide supportive services to the children and mothers within the correctional facility. The collaboration reduced the need for ACCW to develop programs and services specific to the incarcerated population.
The mothers involved expressed great joy and were grateful that they could continue to breastfeed and nurture their babies at the correctional facility. They participated in parenting classes provided by a community agency through visits by the public health nurses and the MCFD worker. They also participated in health examinations by the ACCW physician to ensure the safety and health of their babies. Several of the mothers were permitted to go out into the community on escorted passes, both before and after the birth of their babies, to participate in various programs offered by community agencies that welcomed their participation.
Other women who did not have the opportunity to be with their children had to deal with the reminder of the pain they suffered as a result of being away from their own children. Seeing the babies at ACCW triggered feelings of loss, but a general feeling of hope permeated the entire population and the atmosphere at the facility was more positive in many ways. Incarcerated women wrote about their experiences as part of a prison participatory health research project, and their writing was later published in a book titled Arresting Hope.10
Seeing other ministries and agencies support this initiative had an impact on many of the incarcerated women. Most had very little trust in government agencies due to previous negative interactions. Seeing the agencies working together to ensure the babies stay with their mothers gave them a different perspective from which to view these groups. Some voiced a new interest to work with agencies to initiate contact with their own children with whom they had lost contact, or to work to improve their own lives to make a better life for their children.
For many, seeing the mothers and babies thrive at the facility and be released into the community together continued to reinforce the feeling that this initiative was not only the child’s right but also the right thing to do for the child.
Mother–child unit upheld by BC Supreme Court
In 2008, Brenda retired from ACCW and the BC Corrections Branch Headquarters shut down the prison mother–child unit. Amanda Inglis and Patricia Block, whose babies were born after the unit had closed, became appellants in a five-year legal case that led to a BC Supreme Court hearing in May 2013. During the women’s compelling testimony, Patricia told the court that there were as many as five different people caring for her daughter while they were separated. She tried to continue to breastfeed her baby while in prison, she said, but had difficulties in doing so.
At one point, her daughter’s foster mother stopped using the breast milk that Patricia had pumped because she worried it “wasn’t good milk.” Patricia had to inform the MCFD, who then ordered the foster mother to provide the breast milk to her baby. Patricia said that pumping milk in her prison cell for her newborn baby, who was then staying with relatives, gave new meaning to the phrase “crying over spilt milk.”
In December 2013, Honourable Judge Carol Ross ruled in Inglis v. British Columbia (Minister of Public Safety) that the cancellation of the mother–child unit infringed the Charter right to security of the person (section 7) of the mothers and babies affected by the decision, and that the infringements were not in accord with the principles of fundamental justice. The ruling also held that the cancellation constituted discrimination and violated section 15(1) of the Charter, the right to equality of the members of the affected groups, namely provincially incarcerated mothers who wished to have their baby remain with them while they serve their sentence and the babies of those mothers.
The judge directed the government of British Columbia to administer the Correction Act Regulation in relation to this issue in a manner consistent with the requirements of sections 7 and 15(1), and she gave six months to provide an opportunity for the government to correct the unconstitutionality of the present situation and comply with the Court’s direction.11
Guidelines developed to facilitate program adoption across Canada
The Collaborating Centre for Prison Health and Education (CCPHE) hosted a two-day working meeting in March 2014 at the University of British Columbia to generate best practice evidence-based guidelines to inform the implementation of mother–child units across Canada. Experts were invited to present during four panel discussions entitled “The Rights of the Child,” “The Correctional Context,” “Pathways and Programs” and “Evaluation.”
Thirty stakeholder organizations were invited to contribute to the writing of the guidelines by selecting delegate representative(s) to participate in the working meeting. Delegates included those from BC Corrections Branch, Correctional Service Canada, New Zealand Corrections and Women in2 Healing (formerly incarcerated mothers).
The CCPHE contracted Sarah Payne to write an initial guideline framework based on her analysis of the meeting proceedings. A “content analysis” method was used to ensure that all themes developing from the meeting data were captured in the emergent guidelines. As a final stage, international resources and research publications, which had been presented by experts as evidence during the working meeting, were reviewed.
The resulting Guidelines describe 16 guiding principles and best practices required for optimal child and maternal health inside a correctional facility, including the correctional context, pregnancy, birth, education, correctional and medical care, discharge planning and community partner engagement. Delegates from BC Corrections Branch and Correctional Service Canada, who attended the writing meeting, incorporated the Guidelines’ principles and best practices into their respective organizations’ policies and procedures.
Follow-up evaluations of the mother–child unit currently under way
The ACCW mother–child unit was established on the principle that babies should accompany their mothers back to the ACCW, which was supported by the 2013 BC Supreme Court ruling that deemed it unconstitutional to separate the two. Currently, the “new” BC provincial program and the federal program (as well as programs in the U.S.) are based on the principle that it is a privilege for the incarcerated mother rather than a right: incarcerated pregnant women have to submit an application and go through a difficult, stressful and protracted approval process.
Some infants now currently reside with their mothers in federal women’s correctional facilities across Canada. However, bringing babies to live with their mothers inside provincial correctional facilities has been slow, even though a refurbished mother–child unit opened in July 2014 at ACCW. More education and understanding about the cultural, epigenetic, legal and permanent health impacts of a decision to remove a baby at birth can help support maternal and infant health in prisons across Canada.
A 10-year follow-up evaluation of the ACCW mother–child unit that ran from 2005 to 2007 is currently under way. Through in-depth interviews with mothers whose infants lived at ACCW, this evaluation is exploring their experiences and the current health and social development of their children.
Each of the mothers interviewed to date have reported that the decision to have her baby live with her in prison transformed her life. Each woman attributed the quality and quantity of time that she spent with her baby in ACCW to making a positive long-term impact on the mother–child relationship, and each reported that she now has an exceptionally close relationship with her child. Each woman also spoke very affectionately about her child’s attributes, with kindness and a caring nature as foremost.
Notes
- Ronald R. Abrahams et al., “Rooming-in Compared with Standard Care for Newborns of Mothers Using Methadone or Heroin,” Canadian Family Physician 53:10 (October 2007), http://bit.ly/2k4K29I.
- Marian Knight and Emma Plugge, “The Outcomes of Pregnancy Among Imprisoned Women: A Systematic Review,” BJOG: An International Journal of Obstetrics and Gynaecology 112:11 (December 2005), doi.org/10.1111/j.1471-0528.2005.00749.x.
- Alison Cunningham and Linda Baker, Waiting for Mommy: Giving a Voice to the Hidden Victims of Imprisonment. London, ON: Centre for Children and Families in the Justice System, 2003.
- Helen Fair, “International Profile of Women’s Prisons,” World Prison Brief (February 7, 2008), http://bit.ly/2knx0BM.
- Kiran Bedi, It’s Always Possible: Transforming One of the Largest Prisons in the World. New Delhi: Stirling Paperbacks, 2006.
- Women’s Prison Association, “Mothers, Infants and Imprisonment: A National Look at Prison Nurseries and Community-Based Alternatives,” Institute on Women & Criminal Justice (May 2009), http://bit.ly/2hwPK0L.
- World Health Organization, “Infant and Young Child Feeding,” Fact Sheet (September 2016), http://bit.ly/1o6MEg8.
- Health Canada, “Nutrition for Healthy Term Infants: Recommendations from Birth to Six Months,” A joint statement of Health Canada, Canadian Paediatric Society, Dietitians of Canada, and Breastfeeding Committee for Canada (2013), http://bit.ly/LTH03C.
- Grace S. Marquis, “Breastfeeding and Its Impact on Child Psychosocial and Emotional Development,” Encyclopedia on Early Childhood Development (March 2008), http://bit.ly/1cESBkC.
- Ruth Elwood Martin, Mo Korchinski, Lyn Fels and Carl Leggo, eds., Arresting Hope: Women Taking Action in Prison Health Inside Out. Inanna Publications, 2014.
- Inglis v. British Columbia (Minister of Public Safety), 2013 BCSC 2309 (SC), H.M.J. Ross, http://bit.ly/2jiUVk0.
Dr. Ruth Elwood Martin is a Clinical Professor in UBC’s School of Population and Public Health and recipient of the 2015 Governor General’s Award in Commemoration of the Persons Case.
Brenda Tole is the former warden at the Alouette Correctional Centre for Women from the time it opened in 2004 until her retirement in 2008.
Download this article in PDF format.
Published on February 7, 2017
The Canadian Debate on Spanking and Violence Against Children
Kathy Lynn
Just as families have evolved across generations, so too have our ideas about parenting, children and the social norms regarding discipline. While there is always diversity in what people feel is appropriate, there has been a significant shift across generations away from authoritarian parenting styles toward a more compassionate view that treats children as rights-bearing individuals rather than property.
Despite this societal shift, the use of corporal punishment in the form of “spanking”1 is legally protected under section 43 of Canada’s Criminal Code, also known as the “spanking law.” Section 43 reads as follows:
Every schoolteacher, parent or person standing in the place of a parent is justified in using force by way of correction toward a pupil or child, as the case may be, who is under his care, if the force does not exceed what is reasonable under the circumstances. R.S.C., 1985, c. C-4
This defence first appeared in the Criminal Code in 1892 and has changed little since.2 Discussions about what to do with section 43 have an interesting and active history stretching back to the 1970s and earlier, but it is still on the books today.
“Spanking” in the Courts
Section 43 has been challenged a number of times over the past 30 years. In 1998, the Canadian Foundation for Children, Youth and the Law started a rights-based legal action in the Ontario Superior Court to challenge the constitutionality of section 43 of the Criminal Code on the basis that it violates the Canadian Charter of Rights and Freedoms and the United Nations’ Convention on the Rights of the Child.
The challenge was dismissed by the Ontario Superior Court and the Ontario Court of Appeal. Despite the dismissal, the government argued that physical force should be discouraged as a normative technique of correction. The case then moved on to the Supreme Court of Canada, but, in its January 2004 decision, the Supreme Court held that section 43 did not infringe on the Charter. It did, however, set out a series of judicial limitations (which do not appear in the Criminal Code) on corporal punishment:
- Only parents may use reasonable force solely for purposes of correction.
- Teachers may use reasonable force only to “remove a child from a classroom or secure compliance with instructions, but not merely as corporal punishment.”
- Corporal punishment cannot be administered to children under two or to teenagers.
- The use of force on children of any age “incapable of learning from [it] because of disability or some other contextual factor” is not protected.
- Discipline by the use of objects or blows or slaps to the head is unreasonable.
- Degrading, inhuman or harmful conduct is not protected, including conduct that raises a reasonable prospect of harm.
- Only minor corrective force of a transitory and trifling nature may be used.
- The physical punishment must be “corrective, which rules out conduct stemming from the caregiver’s frustration, loss of temper or abusive personality.”
- The gravity of the precipitating event is not relevant.
- The question of what is “reasonable under the circumstances” requires an objective test and must be considered in context and in light of all the circumstances of the case.3
The current legal context has led to confusion and conflict due to contradictions between the definitions of assault outlined in criminal law and definitions of child abuse found in provincial and territorial law, as outlined by the Ontario Public Health Association:
“… a provincial or territorial child welfare authority may investigate a report of parental physical abuse of a child, conclude that she is at risk in her family and apprehend her. When this happens, police may lay a charge of assault. However, section 43 provides parents with a legal defence against such a charge. This has led to situations which seem to defy logic, in which the definition of “a child in need of protection” in provincial and territorial law leads to the child’s apprehension, but the protection afforded to parents under section 43 of the Criminal Code leads to their being acquitted of assault.”
There have been many legislative attempts to have section 43 repealed or amended, with 17 private member’s bills being tabled in Parliament since 1994, though none have succeeded. Senator Céline Hervieux-Payette has introduced numerous bills; however, to date, all have died at various stages of reading due to elections and prorogations of Parliament.4
Pressure to repeal section 43 has also mounted from the international stage since Canada signed the UN Convention on the Rights of the Child. Article 2 of the Convention states that signatories “take all appropriate measures to ensure that the child is protected against all forms of discrimination or punishment on the basis of the status, activities, expressed opinions, or beliefs of the child’s parents, legal guardians, or family members.”5
In response to reports from Canada regarding the action it has taken to meet the requirements of the Convention, the United Nations Committee on the Rights of the Child recommended that physical punishment of children in schools and families be prohibited and that section 43 be removed from the Criminal Code. However, no action was taken and the law remains on the books. To date, 51 countries have banned the physical punishment of children in all settings.
Most recently, the Truth and Reconciliation Commission (TRC) recommended repealing section 43 as the sixth of its final report’s 94 calls to action. “The Commission believes that corporal punishment is a relic of a discredited past,” it reads, “and has no place in Canadian schools or homes.”6 The federal government has since committed to accepting all calls to action outlined in the TRC report.
“…corporal punishment is a relic of a discredited past, and has no place in Canadian schools or homes.”
– Final Report of the Truth and Reconciliation Commission
“Spanking” Research
A most compelling body of research has been developed around the question of physical punishment of children. In June 2016, Dr. Elizabeth Gershoff, Associate Professor at the University of Texas at Austin, and Andrew Grogan-Kaylor, Associate Professor of Social Work at the University of Michigan, published a literature review that includes a wide range of studies on corporal punishment of children. They found that the research has been consistent. Spanking is at best ineffective and at worst harmful to children.7
A series of meta-analyses have demonstrated that in addition to increases in aggressive behaviour in children, spanking has been associated with increases in mental health problems into adulthood, impaired parent–child relationships, delinquent behaviour and criminal behaviour in adulthood.8 There is also research showing that a risk that initial “corrective” spanking can progress to child abuse.9
The research shows that hitting children is ineffective – instead of teaching children the reasons their behaviour needs to change, it simply causes the child pain and engenders fear. Studies have shown that children need to internalize reasons for behaving in appropriate ways.10 Spanking teaches them to behave in order to avoid physical punishment. When the threat of physical punishment is gone, children find no reason to behave appropriately. Spanking can lead to some children considering violence toward others as a problem-solver. A violent attitude can also work to reduce family cohesion.
The Future of “Spanking” in Canada
Evidence shows that children do not learn appropriate behaviour from being physically hurt. While children need to be accountable for their behaviour, modelling positive behaviours and teaching them to self-regulate, communicate their feelings and ask for help are more effective. Parents play an important role in socializing children, teaching how certain actions and behaviours are not acceptable and providing opportunities to develop the skills to function well in society.
For teaching children to grow and mature into responsible, capable and contributing adults, spanking is not the way. Violence against children should be against the law, not defined by it. We know there are more compassionate and effective ways to raise children to be capable young adults.
Corinne Robertshaw: A Committed Advocate
Corinne Robertshaw was a lawyer with the federal government in the 1970s. She became concerned about injuries and deaths of children caused by parents. She determined that section 43, which provides legal defence for assault against children, was a factor contributing to these injuries and deaths. She produced a study on child deaths caused by physical punishment (Discussion Paper on Child Protection in Canada, February 1981).
In 1990, she retired and dedicated the rest of her life to seeing the repeal of section 43. She created a national, multidisciplinary committee to mobilize Canadians interested in the issue and to continue to develop evidence and arguments in favour of repeal. She died in January 2013 and Corinne’s Quest: End Physical Punishment of Children was formed to continue her work and honour her legacy.
Notes
- The term “spanking” is used in this article to include corporal punishment and the use of “corrective” physical force against children.
- Laura Barnett, “The ‘Spanking’ Law: Section 43 of the Criminal Code,” Parliamentary Information and Research Service (June 20, 2008), http://bit.ly/2d3ZvWi.
- “What’s the Law?” Corrine’s Quest, accessed September 27, 2016, http://bit.ly/2dwYIJ2.
- Coalition on Physical Punishment of Children and Youth, “Physical Punishment Update #16,” Joint Statement on Physical Punishment of Children and Youth (March 2016), accessed September 27, 2016.
- United Nations, “Convention on the Rights of the Child,” Treaty Series (November 20, 1989), http://bit.ly/1fGCcXV.
- Truth and Reconciliation Commission, “Canada’s Residential Schools: The Legacy,” The Final Report of the Truth and Reconciliation Commission of Canada (December 2015).
- Elizabeth Gershoff and Andrew Grogan-Kaylor, “Spanking and Child Outcomes: Old Controversies and New Meta-Analyses,” Journal of Family Psychology, 30:4 (June 2016), doi:10.1037/fam0000191.
- Elizabeth Gershoff, “Corporal Punishment by Parents and Associated Child Behaviors and Experiences: A Meta-Analytic and Theoretical Review,” Psychological Bulletin, 128:4 (July 2002), doi:10.1037//0033-2909.128.4.539.
- Joan Durrant et al., “Punitive Violence Against Children in Canada,” Centre of Excellence for Child Welfare (March 31, 2006), http://bit.ly/2czf1mO.
- Elizabeth Gershoff, “Spanking and Child Development: We Know Enough Now to Stop Hitting Our Children,” Child Development Perspectives 7:3 (July 10, 2013), doi:10.1111/cdep.12038.
Kathy Lynn is a parenting speaker, author and chair of Corinne’s Quest.
This article was reviewed by Rina Arseneault, C.M., Associate Director of the Muriel McQueen Fergusson Centre for Family Violence Research (MMFC) at the University of New Brunswick.
A Snapshot of Workplace Mental Health in Canada
At some point in our lives, we are all affected by mental illness, whether through personal experience or that of a family member, friend, neighbour or colleague. Mental health conditions can have a significant impact on individuals, but they can also “trickle up” to have a detrimental effect on workplaces, communities, the economy and society at large – no one remains untouched. It is therefore vital that support for mental health be multi-faceted and every bit as prevalent as the conditions it seeks to address.
Stigma remains a major barrier to care for those living with a mental illness, many of whom are receiving, and benefiting from, care and support from their families.
This edition of the Vanier Institute of the Family Statistical Snapshots series explores mental health, families and work – three key parts of our lives that intersect and interact in complex ways that affect our well-being.
Highlights include:
- 4 in 10 Canadians have a family member with a mental health problem.
- At least 500,000 employed Canadians are unable to work due to mental health problems in any given week.
- Mental illness accounts for an estimated 30% of all disability claims and 70% of disability costs.
- Stigma remains an issue, with 1 in 5 surveyed Canadian employees saying they believe that whether or not someone becomes mentally ill is “fully within their control.”
- 4 in 10 surveyed Canadian employees say they would not tell their manager if they were experiencing a mental health problem.
- More than 7 in 10 Canadians who are affected by a family member’s mental health problem provided care to them, and 68% say they are not embarrassed about their family member’s mental health condition.
Download A Snapshot of Workplace Mental Health from the Vanier Institute of the Family.
Building Resilience at Home with Distance Coaching
While we all strive to ensure positive mental health and well-being for ourselves and our families, mental health conditions affect most households at some point, directly or indirectly. Children are no exception, with an estimated one in five schoolchildren living with mental health, behavioural or neurodevelopmental disorders.1
Both early intervention and quality, evidence-based care are essential to supporting children with these conditions and building their resilience. For some families, however, it isn’t always possible to access face-to-face intervention services. Lengthy clinic wait times, fear and/or experience of stigma and long travel distances can make it challenging to access appropriate services.
This can be particularly true for military families, in which a parent may have unpredictable schedules that often involve a greater amount of travel, separation, routine disruptions, transitions and overall stress than their civilian counterparts. Due to their high mobility and frequent moves, military families also commonly experience difficulties maintaining continuity of care for their children.2
Flexibility can facilitate mental health care for families
Clinic-based mental health services offer a variety of programs and supports to youth, but many lack the flexibility that families require to support these children while managing other family and work responsibilities. Children’s school schedules often don’t align with available mental health services, and repeated absences due to the need to attend regular appointments at a clinic can have an impact on children’s academic performance and their social relationships with friends and peers.
It may also be difficult or impossible for many parents to take the necessary time off work to bring a child to face-to-face appointments, either because they lack the necessary flexibility at work or because doing so would incur financial hardship. Nearly 7 in 10 couple families with at least one child under 16 have two employed parents, and in three-quarters of these couples, both parents work full-time.3 For single-parent families, the impact of missing work to accommodate appointments can be particularly difficult. Flexibility can be all the more important when seeking support for their children in military families, which often experience high mobility and deployments.
The Strongest Families Institute provides family-centred mental health care
Founded in 2011, the Strongest Families Institute (SFI) is a not-for-profit corporation designed to provide flexible, evidence-based and stigma-free mental health support to children customized to their needs and family realities. Based on six years of research at the Centre for Research in Family Health at the IWK Health Centre in Halifax, Nova Scotia, SFI programs and modules are now accessible across the country. SFI has been nationally recognized for social benefits by the Mental Health Commission of Canada (2012) and was the recipient of the Ernest C. Manning Encana Principal Award (2013).
SFI programs use a family-centred approach, directly engaging and involving family members throughout the process. Families can play a powerful role in facilitating quality mental health care because of their familiarity with the child’s circumstances. They also have a unique ability to provide valuable feedback to service providers throughout the engagement process.
Developing skills to build resilience… from a distance
SFI programs are focused on skill-based learning that fosters mental health and resilience skills through the use of psychologically informed educational modules that help families manage behavioural conditions or difficulties (e.g. not listening, temper or anger outbursts, aggression, attention deficits or hyperactivity) and anxiety (e.g. separation, generalized, social, specific fears).
SFI employs a unique distance coaching approach, utilizing technology to directly support families over the phone and the Internet in the comfort, privacy and convenience of their own home.4 Research has shown that distance coaching can result in significant diagnosis decreases among children with disruptive behaviour or anxiety conditions.5
“[My coach] has taught me a lot of skills that I was not aware of – especially in the conditions of the ever-changing military family life situation – and helped us deal with a lot of challenges. [My child] is more patient and approachable now. He knows how to deal with stress when his father is away [deployed]. His grades and behaviour at school have improved as well, he has fewer outbursts and the teachers have noticed the difference as well.”
– Parent of a 9-year-old participant in the Active Child program (Behaviour)
SFI’s Parenting the Active Child Program focuses on child behaviour for ages 3 to 12. In this program, parents and their children work together to create structured plans to help manage specific challenges a child may experience during particular times or activities. For example, parents and children can work together to develop a plan to make outings such as a trip to the grocery store or long trip in the car more enjoyable by using program skills. Through this simple but structured and guided approach, parents together with their children and the coach can work toward and reward good behaviour. By using the family home as a base for learning rather than a clinic setting, many of the issues of stigma are avoided. Families receive a series of written materials and skill demonstration videos, delivered either through handbooks or by smart-website technology, which teach one new skill per week to implement as part of their daily living activities.
The SFI anxiety program for 6- to 17-year-olds, Chase Worries Away, helps family learn life skills to defeat worries such as separation anxiety, performance issues, social anxiety and specific fears that are commonly related to the challenges of military life. SFI also runs a program for children ages 5 to 12 called Dry Nights Ahead, which helps with nighttime bedwetting.
Coaches ensure stability and guidance throughout the program
Children and families are supported and guided throughout the SFI programs by highly trained and monitored coaches. These coaches engage in structured weekly telephone calls that follow protocolized scripts, complementing the material families receive. During each session, the family’s coach reviews the skill that has been developed throughout the week and uses evidence-based strategies, such as role-playing and verbal modelling, to practise the skills and assess progress.
Schedules are flexible and customizable to accommodate families regardless of where they are located or where they move. This flexibility and focus on distance coaching can be particularly valuable for military families, bridging the geographical divide during separations resulting from postings so that the continuum of care is maintained. Moreover, during a posting, coaches help the families plan for the transition and they remain available during and after to encourage the maintenance of skills. This focus on planning supports families during potentially disruptive transitions, such as during a change of school or daycare.
The coach can be a familiar, centralized contact/support for the family, regardless of the move location. Coaches have high military literacy – understanding of the unique experiences of military families and the “military life stressors” that can have an impact on military families, such as high mobility, extended and/or unexpected separation and risk. Care and support is customized to the realities and needs of each family.
“[The program] helped me quite a bit, especially in everything anxiety, I still have other issues, but in terms of anxiety it has become less of a problem for me, socially, being independent, things I wouldn’t have done before, school stress has reduced quite a bit. They were the main things I was focused toward, and this has decreased stress for me.”
– 16-year-old participant in the Chase Worries Away program (Anxiety)
Transferable learning: Flexible support for diverse and unique families
SFI programs have demonstrated success, with families reporting high satisfaction. Rigorous testing and randomized trials show positive outcomes, with lasting effects one year later, targeting mild and moderate conditions. Programs have been found to have an 85% or better success rate in overcoming the child’s presenting problems, with an attrition rate of less than 10%. Data shows a strong impact on strengthening family relationships, parental mood/stress scores and child academic performance.
Families and their children are unique, and there is no “one-size-fits-all” solution to manage mental health or behavioural or neurodevelopmental disorders. Flexibility in SFI program design and availability can enhance the use and effectiveness of mental health supports, since families can receive support outside of traditional clinic settings and schedules. By using distance coaching and continued family support through structured calls with coaches, families engaged with SFI can receive care that is flexible, effective and respectful of their experiences and realities.
About the Strongest Families Institute
The Strongest Families Institute (SFI) is a national, not-for-profit organization that delivers distance, evidence-based programs to children and families who face issues impacting mental health and well-being. Founded in 2011, SFI seeks to provide timely delivery of services to families when and where they are needed by using technology, research and highly skilled staff.
Over the years, SFI has formed many partnerships to improve its services. Some of these partnerships have helped them deliver services to military and Veteran families, including Military Family Services – Ottawa, Bell True Patriot Love Foundation (Bell Let’s Talk) and a project collaboration with CIMVHR.
Notes
- Ann Douglas, Parenting Through the Storm (Toronto: HarperCollins, 2015).
- Heidi Cramm et al., “The Current State of Military Family Research,” Transition (January 19, 2016).
- Sharanjit Uppal, “Employment Patterns of Families with Children,” Insights on Canadian Society (June 24, 2015), Statistics Canada catalogue no. 75-006-X, http://bit.ly/1Nen7gR.
- Patricia Lingley-Pottie and Patrick J. McGrath, “Telehealth: A Child-Friendly Approach to Mental Health Care Reform,” Journal of Telemedicine and Telecare 14 (2008): 225–26, doi:10.1258/jtt.2008.008001.
- Patrick J. McGrath et al., “Telephone-Based Mental Health Interventions for Child Disruptive Behavior or Anxiety Disorders: Randomized Trials and Overall Analysis,” Journal of the American Academy of Child and Adolescent Psychiatry 50, no. 11 (2011): 1162–72, doi:10.1016/j.jaac.2011.07.013.
Building Inclusive Communities for Canada’s Military and Veteran Families
Col (ret) Russell Mann, OMM, MSM, CD, MBA, PMP
A few decades ago, military families in Canada lived apart from the rest of society. They went to military schools. They practised their faith behind the barbed wire fences of military installations. In many ways, they were a mystery to most Canadians.
But all of that has changed. Whereas 20 years ago, 80% of military families lived on a base, today 85% live off base. Military and Veteran children now attend schools, practise their faith and go shopping alongside civilian families in Canada. They seek health care from the same doctors, family health teams, clinics and hospitals.
For most Canadians, the transition among military and Veteran families from bases to civilian communities has gone largely unnoticed. Now living in civilian communities, these families are neither in the enclave they once knew, nor fully included in the rest of society. Professionals who study, serve and/or support them sometimes fail to understand the impact that mobility, separation and risk have on military and Veteran families.
The transition from military bases to civilian communities is a significant shift for military and Veteran families. It means that the people now serving and supporting them need to be versed in military literacy; it also requires a thorough understanding of their unique lifestyle, perspectives and needs in order to provide these families with effective and equitable programs and services.
Communities rallying to support military and Veteran families
In 2015, the Canadian Armed Forces and the Vanier Institute of the Family partnered to bring government, business and community leaders together to form the Canadian Military and Veteran Families Leadership Circle. The Leadership Circle is unique, and its members are prominent and diverse, including organizations such as the Canadian Child Care Federation, Autism Speaks Canada, Environics Communications, the Mental Health Commission of Canada, Accenture and many more.
This collaboration has a single purpose: to strengthen the community of support for Canada’s military and Veteran families through knowledge mobilization, relationship-building and the coordination of existing and emerging projects and services. By leveraging the skills, talents and expertise of key community leaders, the Leadership Circle is building awareness, capacity, competency and community regarding military and Veteran families in Canada.
“The Leadership Circle has a single purpose: to strengthen the community of support for Canada’s military and Veteran families through knowledge mobilization, relationship-building and the coordination of existing and emerging projects and services.”
The Leadership Circle’s inaugural, first-of-its-kind meeting was held in 2015 to develop a strategy for collaboration, cooperation and communication across the many organizations interested in enhancing programs and services for military and Veteran families, and to develop a shared strategic plan for implementation over the next two to five years.
Discussion at the inaugural meeting focused on sharing individual and collective plans and priorities, goals and objectives, strengths and capabilities, and tools and resources. By the end of that first meeting, participants had a clear understanding of the unique activities and approaches being taken to support military and Veteran families, how they could leverage their collective resources to maximize the outcomes of each individual effort, and how they planned to communicate their progress as the initiative progresses.
During its second annual meeting in 2016, Leadership Circle members committed to creating Military and Veteran Families in Canada: Collaborations and Partnerships – a perpetual, bilingual and free resource that profiles initiatives from diverse organizations across the country. This compendium informs organizations about partnerships and projects, inspires engagement, facilitates resource-sharing and helps coordinate activities to strengthen support for military and Veteran families.
“Organizations profiled in the compendium have incorporated military literacy into their environments, programs and services that serve military and Veteran families.”
One of the goals of the Leadership Circle and the compendium is to enhance military literacy in Canada – awareness of the experiences of military and Veteran families and the unique life stressors (such as mobility, separation and risk) that have an impact on their family life. Organizations profiled in the compendium have incorporated military literacy into their environments, programs and services that serve military and Veteran families exclusively, majorly or occasionally.
Thinking across boundaries facilitates strong networks of support
The Leadership Circle and compendium initiatives have shown us that we can accomplish more and extend our reach by working together. Thinking across organizations and institutional boundaries allows us to see the bigger picture and to mobilize community support across the country. Leadership Circle members are passionate and diverse, and we will continue to discover interconnections and interdependency among stakeholders, service providers and family members; it’s about relationships, and we look forward to helping these relationships grow.
Download Military and Veteran Families in Canada: Collaborations and Partnerships Compendium 1.0.
Colonel (ret) Russell Mann is a former director of Military Family Services. Though recently retired, he continues to champion military and Veteran families.
Sleep and Families
Dr. David B. Posen, M.D.
Sleep is a family affair. When everyone gets what they need, there are benefits for all. When someone is short-changed, it affects everyone else. Research about sleep deprivation is now as compelling as the dangers of smoking 50 years ago, according to Dr. Charles Czeisler, head of the Division of Sleep Medicine at Harvard Medical School, yet many households in Canada are lacking in this vital family resource. This shortage – fuelled by long working hours, new technologies and a 24/7 culture – not only affects productivity at work, performance at school and overall health, but also has a profound effect on families and family life.
What does sleep do for us?
Sleep has many different functions. Sleep is when we restore our physical energy. It’s a time of deep rest and healing, like a “mini-hibernation.” Stress hormones are shut off, heart rate decreases, blood pressure drops, metabolism rate slows and core body temperature falls. It’s when growth hormones are secreted, important for growing children but also contributing to cell repair and replacement in adults. It’s when our immune system is most active, producing T-lymphocytes that fight infection. It’s when hormones affecting hunger and satiety (leptin and ghrelin) are secreted, affecting appetite, food intake and body weight.
Symptoms of sleep deprivation are also symptoms of stress.
Sleep isn’t just important for our bodies, but our minds as well, since it affects mental function. This is when we do our “mental housekeeping,” processing and organizing our previous day’s experiences while discarding irrelevant information (such as what colour sweater someone was wearing on the subway). It is also when we reinforce memory tracks and consolidate new learning. In fact, research shows we actually increase our learning when we sleep.
Symptoms of sleep deprivation are also symptoms of stress. In other words, sleep deprivation shows up in our bodies as stress, in terms of physiological symptoms. When we don’t get enough sleep, cortisol (the main hormone in chronic stress) stays higher longer and has a damaging effect on the body. When we are sleep-deprived, we are less resilient in dealing with stressful situations, less effective problem solvers, less creative and innovative, less affable and can become difficult to get along with.
How sleep (and lack of sleep) affects families
Our sleeping patterns and family lives share a complex relationship, and deprivation affects not just individuals, but families and family systems as well. To examine the impact, let’s first look at cohabiting couples. This usually involves sleeping together, which leads to a number of interesting dynamics that can affect the quantity and quality of sleep a couple receives. When two people share a bed, there are important factors that can affect their sleep that have to be negotiated (or agreed upon), such as the size of their bed, the firmness of their mattress, the temperature of their bedroom and the presence of electronics. Research has shown that light emitted from TVs, smartphones, tablets or light-emitting e-readers can interfere with a good night’s rest.
The time at which one partner goes to sleep or wakes up in the morning can affect the other partner. If a couple has incompatible schedules, both of their sleeping patterns can be negatively affected by the actions and routines of each other. One person may stay up later than they would like because their partner wants to spend more time with them – thus depriving themselves of sleep. Discussion between sleeping partners is crucial to both getting their required amount of sleep. The decisions and agreements made not only affect whether each partner is getting the sleep that they individually need, but also represent negotiations that can either cause conflict in a relationship or provide opportunities for consideration, respect and compromise.
From the start of a live-in relationship to the later stages of our lives, sleep affects members of every family, both individually and collectively.
These are the conscious decisions affecting the bedroom and sleep. But there are involuntary factors as well. One of the biggest disrupters of sleep is a noisy or restless bed partner. The most common issues are snoring and frequent movement in bed. There are many causes of snoring, some mechanical (e.g. sleeping position) and others physiological (e.g. enlarged tonsils and adenoids, large uvula). What’s fascinating is that some snoring can actually reach industrial-strength decibel levels, rattling windows and even disturbing sleepers in other bedrooms – and yet the snorer sleeps through the racket.
Two of the most common sleep disorders are obstructive sleep apnea and restless legs syndrome. With sleep apnea, one of the partners actually stops breathing many times during the night (in fact, many times an hour), often startling themselves awake in order to breathe. Restless legs syndrome causes people to feel discomfort in their legs that is relieved only by continually moving them around, which again can be quite disruptive to the other person in the bed. If this occurs later in life, some couples may decide to move to separate beds or bedrooms to manage their sleep.
A new parent’s life is full of obstacles to sleep
For couples who decide to have children, a whole new variety of factors are brought into the household that affect sleeping patterns and sleep management. This begins with pregnancy. Expectant mothers often have trouble sleeping due to the increasing size of the fetus, the ability to feel the baby moving and increased trips to the bathroom at night. After the baby arrives, disrupted sleep becomes the norm. Babies cry to communicate when they’re hungry, in need of a diaper change or needing to be settled. This can be disruptive to both the new mother (especially if she is breastfeeding) and her partner. This is always a challenging time for getting enough rest, which means it’s an important time for negotiation.
As children get older (around 3 or 4 years of age), they are able to get up and dressed by themselves. Decisions have to be made as to whether a parent gets up with them or whether they train their kids to go to the family room or basement and entertain themselves so their parents can remain in bed. Many parents create a dependency where children expect company and attention from the time they wake up, robbing one or both parents of the extra sleep they need.
Teenagers have a physiological need for more slumber
The next chapter in the parents’ sleep continuum is when children reach early adolescence. This is when something called “phase-shift delay” occurs, where teenagers start to stay up later and then can’t wake up in the morning – a process often misunderstood by parents. Parents often complain that their children are party animals at night (when they won’t go to bed) and then lazy slugs in the morning (when they can’t, or won’t, get up for school). In fact, there’s a biological basis for this. In adults, cortisol levels start to fall at about 10 p.m. and the sleep hormone melatonin is secreted. That’s when we fall asleep. Then, somewhere between 6 and 8 a.m., melatonin secretion stops and we get a surge of cortisol. This allows us to wake up and start our day.
Among teenagers, this whole process is delayed by one or two hours. Cortisol doesn’t shut off and melatonin doesn’t kick in until later in the evening, and the reverse process doesn’t occur until an hour or two later in the morning. Adolescents stay up late because they are not tired yet – it’s physiological. If they don’t wake up in the morning at the same time they used to, it’s likely because their brains are still in “sleep mode” for an extra hour or two. So when they won’t wake up, it’s because they can’t wake up – except with great difficulty.
Teenagers often face a clash between their physiological and academic needs.
Many jurisdictions have moved high school start times to 9 a.m. or even 10 a.m., which is a better biological fit for teenagers. These districts have noticed better attendance at school, improved academic performance and fewer behavioural problems when students are allowed to get the sleep they need in the time frame that corresponds to their physiology. There are also benefits to families from this rescheduling of school hours, as it can reduce morning conflict involved with getting kids up and improve mood and cooperation at home because teens are better rested.
Teenagers often face a clash between their physiological and academic needs. One issue is accomplishing late-night homework and studying for exams. Teenagers are often sleep-deprived (they need nine to 10 hours a night and most are lucky if they get seven), and when you add to that the tendency to stay up well past midnight, finishing assignments or cramming for exams, the problem can become magnified considerably. The more tired they are, the less well they perform on the very tests they stayed up late to study for. Teenagers who also work part-time jobs while going to school face additional challenges, since they must balance school and work with their relatively demanding sleep requirements.
Dr. Stanley Coren, a psychologist at UBC in Vancouver, did a meta-analysis on the effect of sleep deprivation on IQ scores. The results were quite startling. In a newspaper interview, Dr. Coren states that “one hour’s lost sleep out of eight results in a drop of one point of IQ and for every additional hour lost, you drop two points. And it accumulates. So if you cheat on sleep by two hours a night over a five day week, you’ve lost 15 points.”
Functional MRIs show the same thing. With sleep deprivation, electrical activity in the brain decreases. For students who pull all-nighters, by late afternoon the next day, their mental function is significantly impaired and their performance plummets. Even the next morning, their cognitive function is seriously compromised.
Shiftwork creates irregular sleep requirements
Another factor that can have an impact on sleep within families is shift work. I was a family doctor for 17 years, which involved being on call at least once a week, working nights in the ER and being available to deliver babies after midnight. This often involved the phone ringing or my pager going off in the middle of the night, which was disruptive to my wife. The same scenario plays out in families of anyone who has to be available for overnight emergencies – doctors, operating room nurses, hospital technicians, security people or even business owners when there is a security breach at night.
People who work an overnight shift are working against their own physiology.
It also affects people who are regular shift workers, such as police, firefighters, ambulance drivers, paramedics, security guards, factory workers and office cleaners. People who work an overnight shift are actually working against their own physiology. They are being required to be awake at the time when their bodies and brains are biologically programmed for sleeping. After their shift, they go home to try to get some sleep.
This has an effect on everyone in the family, who are then required to maintain as quiet a home environment as possible. This includes everything from limiting or abstaining from radio and TV, phone conversations to spending time indoors with their friends. Any kind of noise might disrupt the sleeping family member who is in desperate need of sleep during the day, when that person’s body is programmed to be awake. The need for other family members to accommodate the irregular sleep requirements of shift work can cause friction, and so discussion, explanation and negotiation are very important.
Sleep requirements change as we age because our bodies change
At the other end of the life-cycle spectrum are circumstances such as menopause for women, where sleep deprivation can be a result of hot flashes or night sweats. As men get older, prostate enlargement often leads to frequent trips to the bathroom at night. People often find it hard to get back to sleep. Many disabilities, which become more prevalent with age, can also affect our sleep, such as shortness of breath due to lung or heart conditions, as well as aches and pains from arthritis, injuries or other musculoskeletal conditions.
Sleep disorders can affect us more as we age. Obstructive sleep apnea becomes more common, especially if a person has gained weight. This is a very underdiagnosed and undertreated condition where sleep deprivation takes a toll. Even though people with sleep apnea may be getting the requisite number of hours in bed and asleep, they are getting the quantity but not the quality of sleep they need. Incidentally, this is where a family member may be an asset: the sleep apnea is often first identified by the partner, not by the patient.
Sleep is a family affair
Sleep is one of the three basic pillars of good health, along with nutrition and exercise. From the start of a live-in relationship to the later stages of our lives, it affects members of every family, both individually and collectively. Awareness of our requirements, and those of other family members, is key to managing our sleep and avoiding the consequences of deprivation. We need to understand sleep so we can talk about and act upon it with serious consideration. Sleep really is a family affair with widespread effects on our physical and mental well-being, and sleep management provides us with opportunities to strengthen our family relationships by being helpful, respectful, understanding and considerate of one another.
Dr. David Posen is a bestselling author (Always Change a Losing Game: Winning Strategies for Work, Home and Health and The Little Book of Stress Relief), international keynote speaker and seminar leader who specializes in stress and change management. His latest book, Is Work Killing You?, explores the relationship between work and well-being.
Work–Family Conflict Among Single Parents in the Canadian Armed Forces
Alla Skomorovsky, PhD
The demands of military life can be particularly stressful for military families due to deployments, relocations, foreign residency, periodic family separations, risk of injury or death of the military member, and long and unpredictable duty hours.
Although military families can usually manage demands individually, research has shown that competing and intersecting demands leave some feeling overwhelmed. This can be particularly true for single parents in the Canadian Armed Forces (CAF), who often manage these multiple roles with fewer resources. This could help explain why enlisted single parents (men and women) have been shown in previous research to be less satisfied with military life than their married counterparts.
Work–family conflict occurs when demands in the work domain are incompatible with demands in the family domain. Despite growing evidence that work–family conflict could be a considerable problem in Canada’s military families, the number of studies examining this topic is relatively small. In a recent qualitative study, the majority of single CAF parents reported that they were able to balance work and family life, but they admitted it was a challenge, primarily because many single parents are often the sole caregivers and financial providers for their families. As one study participant put it,
“So far, the balance between my professional life and my personal life has been quite good. But it’s difficult of course when it’s just me – having to stay late, for example, and still having to work on my phone. I have to have a BlackBerry because I can’t stay late – not as late as I used to anyway. But pretty good, overall.”
Little research exists about work–family conflict in Canada’s military families
Single CAF parents may face multiple deployments and must deal with being separated from their children and not being able to care for them. Caregiver arrangements may be more complicated in these families, as, for example, the children may have to relocate to another city to live with grandparents when their mother or father leaves for a mission. In addition, single parents who experience frequent relocations may find it challenging to establish or re-establish local social networks, which are often a valuable source of support.
A few studies have suggested that single-parent military families have unique military life-related challenges and substantial work–family conflict, but there isn’t much research about this topic in a Canadian context. Director General Military Personnel Research and Analysis (DGMPRA) conducted a study to address this gap and explore the main concerns of single CAF parents. An electronic survey was distributed to a random sample of Regular Force CAF members who had children 19 years of age or younger and were single, divorced, separated or widowed. In total, the results were available for 552 single parents.
Single parents identified financial strain as a top concern; this is consistent with previous research showing that economic hardship is a leading cause of stress for single parents, both military and civilian. The second challenge for single parents was the worry about their child’s health and well-being. Although it has not been previously identified in research of civilian single parents, it is possible that this type of strain was high due to frequent parental absences related to deployment, training, unpredictable/inconsistent hours of work or overtime, common aspects of a military lifestyle. More than 60% of respondents identified financial strain and worry about health and well-being to be of considerable or extreme concern for them (see Figure 1). A large number of these parents (over 50%) were also concerned about dealing with adolescent years, doing the right thing for their children and their heavy demands and responsibilities.
Managing parental and work responsibilities is not impossible, but it is hard
Single parents were asked to rate the extent to which their responsibilities as a service member and as a parent are in conflict. Most do not find it impossible to meet both parental and work responsibilities (see Figure 2). However, about 55% of respondents believe that it is not easy to be both a good parent and service member and feel divided between work and family responsibilities. About 44% of these parents believe it is hard to balance military and parental roles. This is consistent with previous research showing that single military parents are susceptible to experiencing work and family conflict.
Further, participants were asked two questions about family life challenges due to occupational demands. When asked about the influence of work on family life, the vast majority of single military parents reported that work interferes with family life to at least some extent (see Figure 3). Approximately 70% of respondents noted that occupational demands sometimes conflicted with their family life, and 64% disclosed that they had missed family events due to occupational requirements.
In order to examine organizational support available to single parents in greater detail, single parents were asked whether they were aware of CAF programs and policies that could assist them in managing family and work demands. The results demonstrate that many single CAF parents are not aware of services available to them. For example, less than 10% of the participants mentioned that they were aware of Military Family Resource Centre services available to single military parents. This feeling was shared by a participant in the previously-mentioned qualitative study:
“Not everything is well advertised; you need to go and ask. If you are moving to the larger city, look for housing close to a [Military Family Resource Centre].”
Single CAF parents would benefit from work–family supports and greater awareness
Many single CAF parents are thriving, but the work–family conflict remains a considerable concern for some. A qualitative study participant expressed:
“I’m mainly concerned that being in the Canadian Forces may throw something unexpected at me, where I will be left in a position to choose between my career or my children.”
Single CAF parents could benefit from an increased awareness of, and access to, family assistance programs (e.g., Family Care Plans) and other programs, including counselling services. Furthermore, increasing awareness among managers and leaders about the work–family conflict challenges of single CAF parents could foster a more flexible and accommodating work environment. Finally, the ability of these parents to manage work and family responsibilities could be enhanced by tailoring programs and services to single parents (e.g., support groups) in order to increase emotional and instrumental support.
Although this research examines the main challenges and work–family conflict among single-parent CAF families, this is only a first step toward a full understanding of their well-being and unique needs. To further address the current gaps in knowledge, DGMPRA has developed a comprehensive research program related to military families, collaborating extensively with academia (e.g., via Canadian Institute for Military and Veteran Health Research). This body of research seeks to enhance the lives of Canadian military personnel, Veterans and their families. Supporting families is codified in the Canadian Forces Family Covenant, which acknowledges the immutable relationship between the state of military families and the CAF operational capacity.
We recognize the important role families play in enabling the operational effectiveness of the Canadian Forces and we acknowledge the unique nature of military life. We honour the inherent resilience of families and we pay tribute to the sacrifices of families made in support of Canada…
Canadian Forces Family Covenant
Consistent with the Family Covenant, it is important to continue developing the expert knowledge necessary to care for these families and to find ways to best meet their unique needs and ensure their individual and family well-being.
Dr. Alla Skomorovsky is a research psychologist at Director General Military Personnel Research and Analysis (DGMPRA), where she is a leader of the Military Families Research team. She conducts quantitative and qualitative research in the areas of resilience, stress, coping, personality and well-being of military families.
Dr. Skomorovsky received the inaugural Colonel Russell Mann Award for her research on work–family conflict and well-being among CAF parents at Forum 2015 – an event hosted by the Canadian Institute for Military and Veteran Health Research.
This article can be downloaded in PDF format by clicking here.
Suggested Reading
T. Allen, D. Herst, E. Bruck and M. Sutton, “Consequences Associated with Work-to-Family Conflict: A Review and Agenda for Future Research,” Journal of Occupational Health Psychology, 5(2), 278–308 (2000).
G.L. Bowen, D.K. Orthner and L. Zimmerman, “Family Adaptation of Single Parents in the United States Army: An Empirical Analysis of Work Stressors and Adaptive Resources,” Family Relations, 42, 293–304 (1993).
A.L. Day and T. Chamberlain, “Committing to Your Work, Spouse, and Children: Implications for Work–Family Conflict,” Journal of Vocational Behavior, 68(1), 116–130 (2006).
A. Skomorovsky and A. Bullock, The Impact of Military Life on Single-Parent Military Families: Well-Being and Resilience (Director General Military Personnel Research and Analysis Technical Report DRDC-RDDC-2015-R099), Ottawa, ON: Defence Research and Development Canada (2015).
(Still) Eating Together: The Culture of the Family Meal
Paul Fieldhouse
For most Canadians, eating is a daily event so routine, so ordinary that it is taken for granted. But it is also a central part of social relationships and cultural rituals, as well as a symbolic and a material means of coming together. Across cultures and time, food sharing is an almost universal medium for expressing fellowship; it embodies values of hospitality, duty, gratitude, sacrifice and compassion. The shared meal is an opportunity not only to eat, but also to talk, to create and strengthen bonds of attachment and friendship, to teach and learn. Not surprisingly, the family meal is often celebrated as a supremely important component of family life.
The modern family meal
In order to understand “family meals,” it is important to first clarify what the term means. The phrase seems simple enough, but upon examination, the notion of the “family meal” is revealed as convenient shorthand for an idea that may be more imagined than real.
A common image that might come to mind is a happy nuclear family of mom, dad and kids sitting around a nicely laid table enjoying the fruits (and other products) of a largely invisible kitchen production process. Certainly this is an image perpetuated, if not created, by mid-20th-century advertising and popular TV and magazine culture. It has firmly established itself as a cultural ideal, something to be aspired to and emulated – the ultimate symbol of perfect family unity and stability.
It doesn’t take much of a historical read to see that this nuclear concept of the family meal is a fairly modern phenomenon. In Victorian Britain, the children of aristocratic and wealthy families were more likely to eat in the nursery or kitchen with their nanny or the servants, or to eat in communal dining rooms at boarding schools, than to sit at the “family table.” In low-income households, there might not even be a table to sit around.
For young children, “table talk” may be the main source of exposure to family conversation and the expression of thoughts, ideas and emotions.
In North America, “proper” family mealtimes became part of the middle-class consciousness during the second half of the 19th century. During the economic growth and prosperity of the post-war years, the “traditional” idea of the family meal became, perhaps briefly, the norm across social classes.
There are, of course, many types of families and household relationships. What does this mean then for what can be considered a family meal? Does everyone in the family have to be present? Do they have to be eating the same foods? Do they have to be sitting around a table? Does the food have to be prepared from scratch, or at least in the home? Does everyone have to be part of the same household? What if friends or visitors are present – is it still a family meal?
Some attempts to define a family meal include formulas such as at least one adult and one child eating together, two or more people eating together, or members of the same household eating together. Each of these definitions may be necessary but not sufficient to define the family meal and, without common definitions, assessing how common family meals are – and if and how they are changing – becomes very difficult.
The rhythm and role of the family meal
As an everyday ritual, the family meal can be seen as a symbol of shared family life. It organizes the family, regularly bringing family members together and contributing to their physical, mental and social well-being. It provides a rhythm and predictable structure to the day, which can be psychologically reassuring. On the physical or biological level, it is a way to manage the nutritional needs of family members. The extent to which it is successful in so doing depends on a large number of factors, including access to affordable and nutritious food, nutritional knowledge, and food buying and food preparation skills.
The appearance of a meal on the family table represents the outcome of time-consuming and skilled activities that involve both mental decision making and physical work. This work of “deciding and doing,” which applies to all steps of getting a meal, from planning menus to shopping, preparation and serving, is largely invisible and taken for granted.
While this work is still predominantly performed by women, men are increasingly taking on a larger role in family meal preparation than in the past. Cooking a family meal can be an enjoyable and fulfilling task, but it also demands trade-offs in time, money and emotional capital.
With all the work involved, the provision of a family meal is a symbolic demonstration of the care of the meal provider. It may veer more toward love or toward duty, but it always shows commitment to the family group. By sharing meal-related tasks, from shopping to food preparation, table-laying and clearing-up, all family members can participate in this exercise of responsible family solidarity. Failure to do so may be a source of family tension. On the other hand, research has shown that being unable to regularly produce the idealized family meal may provoke feelings of inadequacy and frustration.
Children and teens benefit from family meals
The dinner table is an important place for the socialization of children. The family meal is a prime setting for their introduction to the rules and norms of accepted behaviour and family values and expectations. For toddlers and preschoolers, it teaches what is considered culturally acceptable food and, on a more basic level, what is considered food and non-food.
From a nutritional perspective, family meals provide opportunities for exposing children to a variety of healthy food choices and for modelling healthy eating behaviours, encouraging new tastes and learning to respect appetite as a guide to satiety. But just as healthy choices can be modelled, so can unhealthy ones. If the typical family meal consists of starchy, fatty or high sugar items, with fruit and vegetables making rare appearances, then this pattern will be learned and likely continued.
At family mealtimes, children learn developmental skills, such as holding a cup or manipulating chopsticks, and acquire and develop language and literacy skills through the flow of conversation. For young children especially, “table talk” may be the main source of exposure to family conversation and the expression of thoughts, ideas and emotions.
The lament for the lost family meal may actually be a reaction to perceived or feared change in family structures and arrangements.
Through the exchange of stories, anecdotes and news, children learn about the adult world and the interests and attitudes of their parents, while adults get to learn about the interests and attitudes of their children’s world. At family mealtimes, parents know where their kids are; they can gauge their moods and needs, and uncover and help solve problems.
Research has also suggested that the family meal has a “protective effect.” Children and adolescents who eat more frequently with the family may consume better quality diets and are less likely to be overweight. They have fewer emotional problems and greater academic achievement, and they may be less likely to adopt risky behaviours such as drug and alcohol abuse.
It is not clear what it is about the family meal that is protective. Furthermore, it is difficult to isolate family mealtime from other familial influences. A recent study by two U.S. sociologists suggests that most of the associations between family meals and positive outcomes for youth can be traced to family socio-economic characteristics that make it more likely that they will actually have family meals.
Family meals are changing as families change
Throughout history, the family meal has come to represent the family itself in the public mind, and there is evidence that every generation has lamented its demise. Even in the 1920s, worries were being expressed about how leisure activities and the rise of the car were undermining family mealtimes!
Sociologist Anne Murcott has suggested that the “ideal” is closest to reality among middle-class families, the group that is most anxious about its perceived loss. The family meal represents stability during times of change. The lament for the lost family meal may actually be a reaction to perceived or feared change in family structures and arrangements.
Market research survey polls provide wildly varying data on family meals, making it difficult to draw reliable conclusions. For example, in 2013 a commercial market research company provided a report to their clients that showed eight out of 10 Canadians families had a family meal at least four times a week. In Quebec, this was nine out of 10. In a survey performed for a different client in 2014, the same company reported that only two out of 10 families eat family meals more than twice a week and that 5% of families never had family meals.
While market research data may be contradictory, academic studies and government data on family meals are relatively scarce. Evidence from the U.S., the U.K. and Scandinavia has pointed to family meals happening about half the time. U.S. data for 2003–2013 from the Child Trends Data Bank showed little change in frequency of family meals reported by children, which for six to seven days a week remained at around 55% for 6- to 11-year-olds and 30% for 12- to 17-year-olds. A 2010 U.K. survey suggested that 25% of families ate together nearly every day, while one in 10 families never had an evening meal together and one in five spent less than 10 minutes at the table together.
Instead of mourning the demise of the family meal, we can look for ways to reinvigorate our relationship with food and thus with our families, friends and wider community through intentionally eating together.
Canadian data for the period 1996–2005 showed that workers were spending less time on family activities, including family meals, and were more likely to eat at least one meal alone. The 2010 General Social Survey conducted by Statistics Canada reported that Canadians spent about one-quarter of their waking hours on food-related activities (eating meals at home or at restaurants as well as cooking/washing up), of which 60–70 minutes was devoted to eating meals in the home, with younger people spending the least amount of time on this activity. Another consumer report in 2011 claimed that 55% of Canadians spent 15 minutes or less on preparing a meal.
While this data suggests that time for family meals has diminished, it doesn’t indicate directly whether the number and type of family meals are changing. However, demographic changes in living arrangements are likely to have an impact. In 2011, according to the Canada census, one-person households made up 27.6% of all homes, a threefold increase since 1961 that is especially notable in Quebec.
It is little wonder then that eating alone is becoming common. Recent U.S. polling data suggests that even outside of the home, six out of 10 meals are eaten alone.
What does seem to hold true is that the majority of people still want and value family meals, however they define them. In the U.K. study mentioned above, three-quarters of people wanted to make more effort to sit down together for a family meal. At the same time, many people admit to facing a multitude of barriers in putting this into practice.
Lack of time, work demands, busy social lives, scheduled activities – especially after-school activities for children – and increased opportunities for eating away from home are among the factors militating against the family meal. Lunch has largely disappeared as a family meal, and breakfast may not be far behind as parents report a lack of time to prepare breakfast for their children before school.
People are more inclined to eat when and where they want to in more informal and unstructured ways.
A 2012 workplace consultant report revealed that three in 10 workers don’t take lunch breaks and four in 10 eat alone at their desks. The picture is quite different in France, where the ritual of the shared meal is still a core element of collective everyday life, and in Italy, where three-quarters of the population sit down to lunch in their own homes.
Whereas snacks and mealtimes are spread throughout the day in North America, in France there are three big spikes at morning, noon and night, indicating that traditional meal patterns are strong. At 1 p.m., almost half the French are sitting down to lunch; at 8:15 p.m., more than one-third are having supper. Whether it is a family meal or a meal shared with friends or co-workers, 80% of meals are eaten in the company of others.
Statistics about family meals don’t describe anything about the nature and quality of those events. It is evident that eating patterns are changing in response to changing societal arrangements, including work roles and technology. The concept of set mealtimes to be eaten in the company of specified family members, such as the “three meals a day” pattern familiar to many older people – particularly of European heritage – has largely given way to a less structured, more ad hoc system, aptly described as “grazing.”
At the same time as there are increasing barriers to sit-down, at-home, all-family-members-together meals, food is increasingly available, especially in urban centres, on a 24/7 basis outside the home at restaurants, malls, drive-ins and even non-food outlets, such as big box stores and garden centres. People are more inclined to eat when and where they want to in more informal and unstructured ways.
Future of the family meal
Families may still eat together – though this is often at malls, in fast-food restaurants or in cars en route to the basketball game or dance rehearsal – but to what extent do these constitute family meals? The common elements of food and family are still there, but what may be missing are some of the symbolic and culturally meaningful dimensions of the home-based family meal, some of the cultural learning opportunities and the structure that family mealtimes can bring to the day. When eating in the family car, for example, a parent may not be able to demonstrate the loving and responsible role of provider in the same way, it could be harder for them to teach food manners while in motion and this setting may not invoke the same sense of a refuge from the public sphere or reminder of family unity.
Eating together, whatever and wherever that may be, can help build and strengthen bonds between family members.
Even here, though, care must be taken when making assumptions. Is it not possible to have a conversation about one’s day or to enquire about homework while on the road or sitting around the fast food restaurant table? Some critics have doubted this, yet other studies suggest that when families eat out, they behave in ways very similar to home.
Eating together, whatever and wherever that may be, can help build and strengthen bonds between family members. Perhaps instead of mourning the demise of the family meal, we can look for ways to reinvigorate our relationship with food and thus with our families, friends and wider community through intentionally eating together.
We can take what we believe is good about family meals and put it into practice every time we eat. We can re-envisage mealtimes as a time for conviviality and social bonding. Forsaking the lonely desk lunch and the solo car meal, we can seek out company to share food and community.
Paul Fieldhouse is an adjunct professor in the Department of Human Nutritional Sciences at the University of Manitoba and a nutrition policy and research consultant for the Manitoba government. He has an Interdisciplinary Ph.D. in Food and Religion.
This article is a reprint of (Still) Eating Together: The Culture of the Family Meal, originally published in Transition magazine (Vol. 45 No. 1).
The Current State of Military Family Research
Heidi Cramm, Deborah Norris, Linna Tam-Seto, Maya Eichler, and Kimberley Smith-Evans
Since the 1990s, the nature, frequency, and intensity of military operations have shifted, and these shifts have, in turn, had an impact on the families of Canada’s military personnel. Operational tempo has increased and has been almost continuous, and the roles of Canadian Armed Forces (CAF) personnel1 have changed from “peacekeepers to peacemakers to warriors.” In 2013, the Office of the Ombudsman, National Defence and Canadian Forces released its seminal report on military family health and well-being, On the Homefront: Assessing the Well-being of Canada’s Military Families in the New Millennium. This report brought into view the contexts, meanings, and consequences associated with recent changes in CAF military operations for members, Veterans, and families.
The Ombudsman’s report noted that mobility, separation, and risk have an impact on most serving military members and their families for much of their military careers.2 Canadian military families relocate three to four times more often than their civilian counterparts, with little input as to where, when, or for how long, disrupting continuity of access to health care services. Frequent relocations also affect children’s participation in school, academic progress, and access to educational accommodations for those with identified disabilities or learning exceptionalities.3 Relocations also disrupt non-military family members’ employment opportunities and the family’s capacity to care for vulnerable family members such as aging parents. Protracted separations from family as a result of training or deployment are not uncommon, and the risk that military personnel face during intensive training and deployment speak to the possibility of permanent injury, illness, or death.4 Although Canadian military families value and take pride in their family member’s military service, mobility and separation, along with the “relentless upheaval of military life,”5 can be highly disruptive to families. Civilian family members interviewed for the report shared their concern that their children were “paying a price for their parent’s service to the nation.”6
“…mobility, separation, and risk have an impact on most serving military members and their families for much of their military careers.”
Although Canadian military family research has been ongoing for approximately 25 years, efforts to develop this body of research were, until recently, hampered by the lack of funding for civilian research and the infrastructure to support collaboration. This has recently changed via the networks established through the Canadian Institute for Military and Veteran Health Research. At present, research involving present-day military families focuses overwhelmingly on the US experience. In recent years, this literature has paid greater attention to understanding how military life affects families and how resilience can be enhanced within military families.7 Resilience is defined as “positive adaptation, or the ability to maintain or regain mental health, despite experiencing adversity.”8
“In recent years, [military family research] has paid greater attention to understanding how military life affects families and how resilience can be enhanced within military families.”
On the whole, the research examining military families has tended to take a risk or problem perspective.9 Very little research has explored the factors, or combination of factors, that support successful and ongoing resilience within military family life.10 Little is known about the mechanisms that foster resilience. Instead, emphasis has been placed on the effects of deployment across mental health, social, academic, and behavioural domains.11–14 For example, the mental health of both the deployed and the at-home parent can affect children at different times. The Children on the Homefront study in the United States, which explored the impact of military operations on children’s well-being, described how the mental health of the non-deployed parent had a significant impact on the number of emotional, social, and academic challenges children experience both during deployment and during the reintegration of the deployed parent.15 A recent report that reviewed the Canadian and international research on the impact of operational stress injury (OSI) on family health and well-being16 suggested that it has a negative impact on family dynamics and the health and well-being of family members. Furthermore, it appears that family members experience more emotional, psychological, behavioural, social, and academic problems and are also more vulnerable to experiences of neglect or abuse than other families.17
“…the mental health of both the deployed and the at-home parent can affect children at different times.”
The extent to which these research findings resonate with the Canadian experience is unclear. Canadian military families, especially those who are not actively serving, express “concern that relatively little is known on the subject from a Canadian context.”18 Although many of the findings may be generalizable to Canada, critical differences require more extensive and intensive knowledge of the unique needs of Canadian military children, spouses, and families.19 For instance, in Canada, unlike in the United States, military families are dependent on the civilian health care system and need to repeatedly navigate access to a family doctor as well as any required specialists, often across provincial jurisdictions in which systems and eligibility for services may differ. Rather than enjoying continuity of care, members of military families find themselves on new wait lists with each move, with limited ability to engage in routine health maintenance with a regular health provider. Many Canadian military families travel back to their physician from their previous posting because they have been unsuccessful in securing one in their current residence. If members of the family have medical needs or disabilities, navigating new health care systems can be onerous and frustrating, with eligibility and reimbursement policies causing considerable stress. This can be complicated if civilian health care providers have “limited understanding of the particularities of military life, which can also impact care quality and continuity.”20
The challenges military families face in navigating the health system can be echoed in the school systems. Twenty years ago, 80% of CAF families lived on base and attended a Department of National Defence school there. Not only does that school system no longer exist, 85% of CAF families now live off base and attend community schools21 in which civilian personnel have little awareness of military life stressors and their impact on spouses and children. Moreover, unlike the United States or the United Kingdom, Canada has no federal government department that provides financial resources to provincial school districts to tailor programming for children in military families transitioning into their schools, experiencing parental deployment, or living with a parent with an OSI.22, 23 If a student has a disability and requires educational accommodations in school, the assessment and resource allotment process begins anew with each school transition, which creates significant stressors for families.24
“…it is critical that unique health issues and needs be carefully defined and understood in a Canadian context.”
Although programming and services have been developed in Canada to target families, including crisis support, peer support, psychoeducation, and counselling services through organizations such as the Military Family Resource Centres (MFRCs), offerings vary by location and centre. Canada has also demonstrated leadership in developing family-centred programs and services such as “The Mind’s the Matter” webinar series for adolescents.25 The extent to which most of these programs and services have been based on evidence or rigorously evaluated for efficacy is unclear, however.
To ensure that the spouses and partners of military members and the almost 64,100 Canadian children growing up in military families enjoy the same levels of health as their civilian counterparts, it is critical that unique health issues and needs be carefully defined and understood in a Canadian context. Although clarifying these needs is critical, research must also explore the knowledge and skills that educators, health care practitioners, and community partners require to effectively engage and support military families and ultimately create the foundation for evidence-informed interventions and programming.
Authors
Heidi Cramm, School of Rehabilitation Therapy, Queen’s University, Kingston, ON
Deborah Norris, Department of Family Studies and Gerontology, Mount Saint Vincent University, Halifax, NS
Linna Tam-Seto, School of Rehabilitation Therapy, Queen’s University, Kingston, ON
Maya Eichler, Department of Political and Canadian Studies, Mount Saint Vincent University, Halifax, NS
Kimberley Smith-Evans, Department of Family Studies and Gerontology, Mount Saint Vincent University, Halifax, NS
This article can be downloaded in PDF format here.
This article is an excerpt from “Making Military Families in Canada a Research Priority,” which includes a discussion about future research priorities. The original article, published online in the Journal of Military, Veteran and Family Health in November 2015 (Volume 1 No. 2), can be accessed on the journal’s website.
REFERENCES
- Ombudsman Department of National Defence and Canadian Forces. On the Homefront: Assessing the Well-being of Canada’s Military Families in the New Millennium. Ottawa: Office of the Ombudsman, National Defence and Canadian Forces, 2013.
- Ibid.
- Bradshaw CP, Sudhinaraset M, Mmari K, et al. “School Transitions Among Military Adolescents: A Qualitative Study of Stress and Coping.” School Psych Rev. 2010;39(1):84–105.
- Ombudsman Department of National Defence and Canadian Forces.
- Ibid.
- Ibid.
- Saltzman WR, Lester P, Beardslee WR, et al. “Mechanisms of Risk and Resilience in Military Families: Theoretical and Empirical Basis of a Family-Focused Resilience Enhancement Program.” Clin Child Fam Psychol Rev. 2011;14(3):213–30.
- Herrman H, Stewart DE, Diaz-Granados N, et al. “What Is Resilience?” Can J Psychiatry. 2011;56(5):258–65. Medline: 21586191
- Easterbrooks MA, Ginsburg K, Lerner RM. “Resilience Among Military Youth.” Future Child. 2013;23(2):99–120. Medline: 25518694
- Palmer C. “A Theory of Risk and Resilience Factors in Military Families.” Mil Psychol. 2008;20(3):205–17.
- Aronson KR, Perkins DF. “Challenges Faced by Military Families: Perceptions of United States Marine Corps School Liaisons.” J Child Fam Stud. 2013;22(4):516–25.
- Cederbaum JA, Gilreath TD, Benbenishty R, et al. “Well-Being and Suicidal Ideation of Secondary School Students from Military Families.” J Adolesc Health. 2014;54(6):672–7. Medline: 24257031
- Cozza SJ. “Children of Military Service Members: Raising National Awareness of the Family Health Consequences of Combat Deployment.” Arch Pediatr Adolesc Med. 2011;165(11):1044–6. Medline: 21727261
- Chandra A, Lara-Cinisomo S, Jaycox LH, et al. “Children on the Homefront: The Experience of Children from Military Families.” Pediatrics. 2010;125(1):16–25. Medline: 19969612
- Ibid.
- Norris D, Cramm H, Eichler M, Tam-Seto L, Smith-Evans K. “Operational Stress Injury: The Impact on Family Mental Health and Well-being. A Report to Veterans Affairs Canada.” 2015.
- Ibid.
- Ombudsman Department of National Defence and Canadian Forces.
- Dursun S, Sudom K. “Impacts of Military Life on Families: Results from the Perstempo Survey of Canadian Forces Spouses.” Ottawa: Defence R&D Canada, 2009.
- Ombudsman Department of National Defence and Canadian Forces.
- Military Family Support Services. Canadian Forces Morale and Welfare Services; n.d. [cited 2015 Sep 10]. “Debunking Myths: The Canadian Forces Family Lifestyle.”
- Ombudsman Department of National Defence and Canadian Forces.
- National Military Family Association. Department of Defense Support to Civilian Schools Educating Military Children. Alexandria (VA): The Association, 2006.
- Ombudsman Department of National Defence and Canadian Forces.
- Military Family Support Services. Canadian Forces Morale and Welfare Services; n.d. [cited 2015 Sep 10]. “The Mind’s the Matter: Understanding a Family Member’s OSI.”
Modern Motherhood: The Unique Experiences of Women with Physical Disabilities
Lesley A. Tarasoff
There is very little research concerning pregnancy, labour, birth and motherhood among women with physical disabilities and women with disabilities more broadly. While most women face a variety of social and emotional pressures to have children, research has found that women with disabilities have a very different experience, as they are often pressured not to have children. Many of these girls and women experience “training against motherhood” as soon as they are diagnosed as having a disability. Despite these pressures, there are many women with physical disabilities who are also mothers. Although in Canada it is difficult to determine just how many women with physical or mobility-limiting disabilities are mothers, data from the United States suggests that they are becoming mothers at similar rates to women without disabilities.
As part of a long-term project, a diverse group of women with physical or mobility-limiting disabilities in the Greater Toronto Area have been interviewed about their experiences during the perinatal period – pregnancy, labour, birth and early motherhood. Drawing on other research studies and preliminary findings from this project, this article looks at some of the unique experiences of women with physical disabilities during the perinatal period.
While most women face a variety of social and emotional pressures to have children, research has found that women with disabilities are often pressured not to have children.
There are many misconceptions about women with physical disabilities, including the idea that they cannot or should not become mothers. Women with physical disabilities are often on the receiving end of disability and reproductive “microaggressions.” Initially conceptualized with regard to racial and ethnic minority groups, microaggressions refer to “the brief and commonplace, daily verbal, behavioral, and environmental indignities, whether intentional or unintentional, that communicate hostile, derogatory, or negative … slights and insults on the target person or group.” Disability or ableist microaggressions include things such as exclusion, messages of undesirability, messages of burden, assumptions, pity and astonishment (e.g., the realization that a person with a disability is capable of achievements).
For women with disabilities who are pregnant or who are mothers, these ableist beliefs and patterns of behaviour are often compounded with what some call reproductive microaggressions. These can be direct, such as denying privacy by asking when a woman will have a baby, or indirect, such as expressions of gratitude for having a “healthy child.” Underlying many reproductive microaggressions is reproductive privilege (i.e., the traditional idea or ideal of which women should be mothers [read: white, middle-class, heterosexual, women without physical disabilities]), together with the idea that motherhood is the most exalted form of identity for women.
Jane, one of the research project participants – a married and employed mother of two with a spinal cord injury – shared her thoughts about her perinatal experience. While it was positive overall, largely thanks to her strong advocacy skills and a great team of health care providers, she still experienced a number of negative social interactions commonly experienced by women with physical disabilities in the perinatal period. Sometimes these interactions were overtly discriminatory and negative, such as when a stranger on the sidewalk told her she “shouldn’t be allowed to have children.” Other times, the microaggressions were less explicit. Like many women with physical disabilities, Jane found that many people didn’t see pregnancy as a possibility for her or recognize her as being pregnant as they might have with other women. She often encountered subtle reactions of surprise (astonishment) to her pregnancy and status as a mother while in public spaces such as waiting rooms. Sometimes the microaggressions she described took the form of differential treatment, such as the time she was asked in a grocery store whether she had her daughter “naturally” – noting that it’s unlikely a mother without a disability would have been asked the same question.
Research suggests that women with physical or mobility-limiting disabilities are becoming mothers at similar rates to women without disabilities.
Microaggressions at the intersection of disability and reproduction can also take the form of denying identity or personality by asking a mother without disabilities “Is that your baby?” or of desexualizing women with disabilities through comments such as “I can’t believe you have a baby.” These comments were occasionally directed at Jane, who said that many people she encountered assumed that she had adopted. Microaggressions sometimes take on a patronizing form, such as when people say they feel “inspired” by women with disabilities who decide to have children. Finally, microaggressions also include assumptions of helplessness and infantilizing remarks directed at these mothers, such as asking “Do you need help with your baby?”
Despite the assumption that spinal cord-injured women are able to give birth only via Caesarean section, research reveals that they can have vaginal births. “Everyone still thinks that I had a C-section,” says Jane, acknowledging this misconception.
Indeed, a growing body of research indicates that many women with physical disabilities experience fertility no differently than their counterparts without disabilities and they are capable of becoming pregnant and experiencing vaginal delivery. Though limited, there is some research concerning the pregnancy outcomes of women with physical disabilities. Some of this research suggests that expectant mothers who have physical disabilities may experience common symptoms of pregnancy more severely, and that pregnancy can temporarily or permanently “alter the course” of the disability.
Perinatal outcomes among women with physical disabilities vary depending on the type and severity of their disability. “As much as I want to say that my pregnancy was the same as everyone else’s,” Jane says, “I do admit that there probably were higher risks of complications with mine to a certain degree.” For instance, she noted that her mobility worsened during the course of her pregnancy – a change that she says wasn’t fully recognized by care providers. Indeed, studies reveal that health care providers generally do not know a great deal about the interaction of pregnancy and disability. Jane cited an example of her nurses not knowing a lot about the different catheter options.
Likewise, many of the women with physical disabilities who were interviewed, including Jane, reported feeling frustrated with the lack of perinatal information available to them and often experienced feelings of isolation because it was difficult to find others to share their experiences with. “I found it very frustrating that there is so little research. So any question I had, nobody could give me an answer,” she says. “It was always like, ‘We don’t really know. We’re not really sure.’” In addition to informational barriers, many women with physical disabilities report encountering inaccessible care settings. Jane cited examples such as places with bathrooms or showers she couldn’t access or fit her wheelchair into.
Disabled or not, at one time or another, everybody needs assistance, and it is rare that someone really, truly raises a child single-handedly.
Exploring how women with physical disabilities experience the perinatal period will provoke an interrogation of the self, of what is “normal” and what accessibility is, as well as what independence looks like. Parents with disabilities, like all parents, are creative and adaptable. In many cases, formal resources and supports are not available or accessible, and so some parents with disabilities may rely on unconventional resources and other supports to fulfill their roles effectively. At one time or another, everybody needs assistance whether they have a disability or not, and it is rare that someone really, truly raises a child single-handedly.
Moreover, for some mothers with physical disabilities, becoming a parent takes focus away from their disability and places it on other aspects of their lives, such as the new bond between parent and child as well as the child’s imagination and creativity. As Jane puts it, “Becoming a mom is probably the best thing that I did because it totally lessened … my focus or other people’s focus on my disability. My parents ask way less about my own health; they ask more about the kids.”
In particular, Jane talked about how her physical inability to do certain activities with her young son has led to opportunities to bond and play with him in other ways:
“[My son] knows that I do all the creative stuff with him, so I do all the artwork… he kind of sees us [my husband and me] as having those different [roles] … I love doing imaginative things and I think that’s important for his growing and learning … so for me what’s really boosted my confidence in parenting is that I have that ability or that gift to do that with him and the daycare has commented that he’s such a really imaginative kid…”
A number of other mothers who were interviewed shared similar stories about their relationships with their children and talked about how becoming a mother enhanced their confidence.
Many of the mothers also worried about how their children might be treated in school when other children found out that their mother has a disability: “Kids can be mean… I don’t want people to make fun of him because of me.” One mother with a congenital condition that often limits her mobility, as well as causes hearing and vision problems, arthritis and chronic pain, noted, however, that she uses her disability as a learning opportunity for her young son: “I don’t want him to make fun of anybody. I am trying to tell him that everyone is different.”
The experiences of women with physical disabilities during the perinatal period, including their parenting experiences, provide learning opportunities for all families and their children. This ongoing research project will help to develop resources for women with physical disabilities and health care providers and shed light on some of the positive experiences that they have during the perinatal period. Listening to and documenting the stories and experiences of women like Jane will be integral to this process of providing support.
Lesley A. Tarasoff is a Ph.D. candidate in Public Health at the University of Toronto. She conducts research in the area of women’s sexual and reproductive health, with a focus on women with physical disabilities and sexual minority women. For more information about her research, visit www.latarasoff.com.
Learn more:
Lesley A. Tarasoff, “We Don’t Know. We’ve Never had Anybody Like You Before”: Barriers to Perinatal care for Women with Physical Disabilities,” Disability and Health Journal 10:3 (July 2017). Link: http://bit.ly/2fmk65C.
Lori E. Ross, Lesley A. Tarasoff, Abbie E. Goldberg and Corey E. Flanders, “Pregnant Plurisexual Women’s Sexual and Relationship Histories Across the Life Span: A Qualitative Study,” Journal of Bisexuality (August 11, 2017). Link: http://bit.ly/2wfhZaN.
Lesley A. Tarasoff, “Experiences of Women with Physical Disabilities during the Perinatal Period: A Review of the Literature and Recommendations to Improve Care,” Health Care for Women International 36:1 (July 2013). Link: http://bit.ly/2hqbiQE.
Update: In September 2017, a community report was published based on this research into the experiences of women with physical disabilities. “Becoming Mothers: Experiences of Mothers with Physical Disabilities in Ontario” is now available to download on Lesley’s website.
SOURCES
Judith Rogers, The Disabled Woman’s Guide to Pregnancy and Birth (New York: Demos Medical Publishing, 2006).
Corbett Joan O’Toole, “Sex, Disability and Motherhood: Access to Sexuality for Disabled Mothers,” Disability Studies Quarterly 22:4 (2002).
Lisa I. Iezzoni, Jun Yu, Amy J. Wint, Suzanne C. Smeltzer and Jeffrey L. Ecker, “Prevalence of Current Pregnancy Among US Women with and without Chronic Physical Disabilities,” Medical Care, 51:6 (June 2013).
Alette Coble-Temple, Ayoka Bell and Kayoko Yokoyama, The Experience of Microaggressions on Women with Disabilities: From Research to Practice and Reproductive Microaggressions and Women with Physical Limitations. Presentations at the American Psychological Association Annual Convention (August 2014).
Derald Wing Sue, Jennifer Bucceri, Annie I. Lin, Kevin L. Nadal and Gina C. Torino, “Racial Microaggressions and the Asian American Experience,” Cultural Diversity and Ethnic Minority Psychology, 13:1 (2007).
Ayoka K. Bell, Nothing About Us Without Us: A Qualitative Investigation of the Experiences of Being a Target of Ableist Microaggressions (2013 doctoral dissertation), retrieved from ProQuest Dissertations and Theses (dissertation/thesis number 3620204).
Heather Kuttai, Maternity Rolls: Pregnancy, Childbirth and Disability (Fernwood Publishing, 2010).
Caroline Signore, Catherine Y. Spong, Danuta Krotoski, Nancy L. Shinowara and Sean Blackwell, “Pregnancy in Women with Physical Disabilities,” Obstetrics & Gynecology, 117:4 (2011).
Suzanne C. Smeltzer and Nancy C. Sharts-Hopko, A Provider’s Guide for the Care of Women with Physical Disabilities and Chronic Health Conditions (2005).
Published on December 3, 2015
Updated on September 25, 2017
The Online Lives of Canadian Youth
Matthew Johnson
November 2–6 is Media Literacy Week, an event that highlights the importance of teaching children and teens digital and media literacy skills to ensure their interactions with media are positive and enriching. In this week’s blog post, Matthew Johnson from MediaSmarts discusses the online behaviour of Canadian youth and the role of parents in their lives on the Web.
Digital natives. Tech-savvy. Narcissistic. Innovative. Mean. There are a lot of assumptions about kids online, but the labels we use are often misleading and out of step with what young people are actually doing with networked technologies. In order to better understand the online lives of Canadian children and youth, MediaSmarts – a Canadian not-for-profit charitable organization for digital and media literacy – conducted an extensive national survey of students in Grades 4 through 11 as part of the Young Canadians in a Wired World research series, which began in 2000.
It goes without saying that eight years is a long time on the Internet. Between 2005, when MediaSmarts published Phase II of its Young Canadians in a Wired World research, and 2013, when it conducted the national student survey for Phase III, the Internet changed almost beyond recognition: online video, once slow and buggy, became one of the most popular activities on the Web, while social networking became nearly universal among both youth and adults.
Young people’s online experiences have changed as well, so MediaSmarts surveyed 5,436 Canadian students in Grades 4 through 11, in classrooms in every province and territory, to find out how. The first report drawn from this survey, Life Online, focuses on what youth are doing online, what sites they are going to and their attitudes toward online safety, household rules on Internet use and unplugging from digital technology.
Nearly all youth have access to the Internet
One finding, which is unlikely to be a surprise, is that nearly all youth are going online. In fact, 99% of students surveyed have access to the Internet outside of school using a variety of devices. The biggest change since the last survey is the proliferation of mobile and portable devices, such as tablets, smartphones and web-enabled MP3 players, which give youth constant – and often unsupervised – online access. In the previous Young Canadians in a Wired World report, in 2005, the majority of students accessed the Internet through shared desktop computers at home (which were often kept in the family room or kitchen so parents could keep an eye on the online activities of their children), whereas now portable and personal networked devices, such as tablets and smartphones, are the primary access point for many of these students.
Portable, private access to the Internet was found to increase with age, while reliance on shared computers has decreased: 64% of Grade 4 students report using a shared family computer to go online outside of school, but this drops to 37% by Grade 11. Ownership of cellphones and smartphones, on the other hand, is reported by 24% of students in Grade 4, 52% of students in Grade 7 and 85% of students in Grade 11. Perhaps not surprisingly, ownership of these devices is correlated with family affluence: a greater proportion of more-affluent students compared with medium-affluent students report access to portable computers (74% vs. 61%), cellphones (49% vs. 41%) and game consoles (45% vs. 38%).
Not only are students getting connected, they are staying connected: more than one-third of students who own cellphones say they sleep with their phones in case they get calls or messages during the night. This is true of both girls and boys (39% and 37%, respectively, of those who own cellphones). The trend increases across grades to peak at just over half (51%) of Grade 11 students, but one-fifth of all students in Grade 4 also report that they do the same.
Students are well aware that they are frequently “plugged in”: 40% of girls and 31% of boys report worrying that they spend too much time online. When asked how they would feel if they could not go online for anything other than school or work for a week, just under half (49%) say they would be upset or unhappy. Interestingly, English-language students outside of Quebec are more likely to be upset than French-language students in Quebec (51% vs. 40%). However, 46% of all students indicate they would not care one way or the other and 5% report that they would be relieved or happy to go offline.
Many students try to balance their online and offline activities, saying that they sometimes choose to go offline in order to spend more time with friends and family (77%), go outside or play a game or sport (71%), read a book (44%) or just enjoy some solitary quiet time (45%). Only 4% say that they never choose to go offline to do any of these things.
Youth go online to learn, play games and socialize
What are Canadian youth doing when they are online? For many, the Internet is a tool for learning and sharing information: half (49%) of students in all grades have gone online to find information about news and current events and half of students in Grades 7–11 have sent links to news stories or current events to others. However, relatively few have participated in online debates, either by posting comments on a news site (71% of Grades 7–11 have never done so) or joining an activist group (65% of all grades have never done so).
Students report looking for information on the Internet on sensitive topics, such as mental health issues, sexuality, physical health issues and relationship problems.
Children and youth are not just interested in learning about news and current events, however. Many report going online to learn about health and well-being, whether it’s to learn about physical health (20% of girls and 16% of boys), mental health (14% of girls and 9% of boys) or relationship problems (18% of girls and 9% of boys). The percentage of students who use the Internet as an information source increases from Grade 4 through to Grade 11.
Compared with students in younger grades, a higher percentage of students in Grades 7–11 report looking for information on more sensitive topics, such as mental health issues, sexuality, physical health issues and relationship problems. However, nearly one-quarter (22%) of students report that they do not use the Internet to find information about any of these things. Close to one-third of students report having gone online to ask an expert (30%) or other kids (33%) for advice about a personal problem, although only a small percentage report frequently doing so.
Two-thirds of students report that they play online games, with this activity being significantly more popular among boys (71%) than girls (47%). Unlike other online activities, which increase with age, the proportion of students who report playing online games decreases over time, from a high of 77% in Grade 5 to a low of 42% in Grade 10.
Not surprisingly, social networking is also a popular activity, particularly among older students in the survey. The increased participation in social media-related activities is consistent with developmental literature that suggests that social connection becomes more important as young people move from childhood to their teen years. Between Grade 4 and Grade 11, reading others’ profiles increases from 18% to 72%, tweeting increases from 5% to 42%, following friends/family on Twitter rises from 8% to 39%, posting on one’s own profile rises from 19% to 50% and following celebrities on Twitter rises from 5% to 32%. Girls are more likely than boys to report using social media to communicate with family and friends (45% posted on their own social networking site, compared with 36% of boys).
Many parents regulate the online lives of their children
Parents have continued to be involved in their children’s online lives, with 84% of surveyed students reporting that they have household rules to follow regarding their online activity. The most common rules are about posting contact information online (55%), talking to strangers online or on a cellphone (52%), avoiding certain sites (48%), treating people online with respect (47%) and getting together with online acquaintances (44%).
There have been changes involving household rules regarding online activities since the 2005 survey. Although MediaSmarts’ 2012 focus groups with parents and youth showed parents were more concerned than ever about what youth were doing online, the average number of household rules has actually declined since 2005. For example, in the earlier survey, 74% of students had a rule at home about meeting people whom they first met online, compared with only 44% today. Regarding personal information, 69% of students in 2005 had a rule about giving personal information online, whereas 55% in 2013 had a rule about posting contact information.
84% of surveyed students report that they have household rules to follow regarding their online activity.
Consistent with our previous research, household rules have a significant positive impact on what students do online, reducing risky behaviours such as posting contact information, visiting gambling sites, seeking out online pornography and talking to strangers online. In general, though, the number of household rules takes a sharp dive after Grade 7 and at all ages girls are more likely to report having rules about their online activities than boys. For example, girls are more likely than boys to report having online rules about talking to strangers (61% of girls vs. 40% of boys), getting together with someone they have met online (52% vs. 35%), telling their parents about anything that makes them uncomfortable online (46% vs. 30%) and treating people online with respect (54% vs. 40%).
The greater number of rules placed on girls may be based on a sense that girls are generally more vulnerable, but it may also relate to the fact that the Internet is a very different place for girls than for boys. Girls are less likely to agree with the statement “The Internet is a safe place for me” and more likely to agree that “I could be hurt if I talk to someone I don’t know online.” Despite these differences, both boys and girls feel confident in their ability to look after themselves, with nine out of 10 agreeing with the statement “I know how to protect myself online.”
Youth learn about online life from a variety of sources
Students do see their parents as a valuable resource for learning about the Internet: nearly half (45%) of students say they have learned about issues such as cyberbullying, online safety and privacy management at home. However, parents aren’t their only source of information about online issues, with students also reporting learning about these issues from teachers (41%), friends (18%) and online sources (19%). As students get older, they are less likely to report having learned about these issues from parents and more likely to learn from teachers: for example, students in Grades 4–6 were more likely to report having learned about how to be safe online from parents (75%) than teachers (50%). A worrying number of students have not learned about these topics from any source. For example, more than half of students in Grades 4–6 have not learned any strategies for authenticating online information either at home or at school.
Life Online has raised many issues that call for more in-depth study. However, the evidence is clear at this early stage that despite their confidence with digital tools – or perhaps because of it – Canadian youth, and particularly elementary-aged children, need instruction in digital literacy skills, and parents and teachers need to be given tools and resources to help them provide that instruction.
This article was originally featured in Transition magazine in fall 2013 (Vol. 43, No. 3).
Matthew Johnson is Director of Education at MediaSmarts, Canada’s centre for digital and media literacy.
For resources and information about digital and media literacy, visit the MediaSmarts and Media Literacy Week websites.
When Cupboards Are Bare: Food Insecurity and Public Health
Nathan Battams
(Updated September 6, 2017)
Food security is an issue that is deeply intertwined with the health and economic well-being of families. It is a serious social, economic and public health concern, felt not only by the estimated 1.3 million households in Canada that reported experiencing food insecurity in 2014 (12% of households, home to 3.2 million people), but also by the communities in which they live. When families face obstacles in securing the quantity and quality of meals they need to thrive, it becomes all the harder for them to be healthy and live productive, happy lives.
When the Canadian Medical Association consulted Canadians about public health issues in a series of town hall meetings in 2013, food insecurity was identified as one of the main social determinants of health. Without a stable and healthy food supply, people are more likely to develop a range of health issues, such as heart disease, diabetes, stress and even food allergies.
While there are multiple contributing factors to food insecurity, including geographic isolation, food literacy and transportation issues, economic insecurity is at the heart of the matter.
Since the beginning of the Great Recession in 2008, families have increasingly depended on food banks and other community supports for essential support securing the quantity and quality of food they need. According to Food Banks Canada, the number of people who accessed food banks across the country in March 2016 (863,492) was 28% higher than in 2008, and more than 40% of households receiving food were families with children.
Some individuals are more likely than others to experience food insecurity. Food insecurity rates were higher than the national average in 2014 for people with an Aboriginal identity (26%) and for Black people (29%). A 2016 study also found that some households are more likely than the national average to experience food insecurity, including (but not limited to):
- Households with children under age 18 (15.6% versus a 10.4% food insecurity rate for households without children)
- Lone-parent families headed by women (33.5%)
- Households in Nunavut (60%)
- People living in rented households (25%)
- Households with an income below the Low Income Measure (29.2%)
Research from Statistics Canada has suggested that adults experience food insecurity at higher rates than children (8.2% compared with 4.9%) because parents are protecting their youngsters from food insecurity by reducing the variety and quantity of their own meals so their children can eat better. Despite this, children across Canada are affected by food insecurity, with children and youth accounting for 36% of those helped by food banks in March 2016.
Food banks and community supports were never intended to be permanent solutions to food insecurity. Many organizations providing food to families are feeling the pressure resulting from the economic downturn. Faced with increased demand, some food banks have had to reduce the assistance they provide – a reality with serious consequences for the health and well-being of families in Canada.
There are multiple contributing factors to food insecurity, including geographic isolation, food literacy and transportation issues, but economic insecurity is at the heart of the matter. Families can’t eat when they don’t have the power to buy. Rates of food insecurity vary widely across Canada, reaching as high as 47% in Nunavut and the Northwest Territories in 2014. Some people face disproportionately high rates of low income, such as sole-support mothers and Indigenous people, and are therefore also more likely to experience higher levels of food insecurity.
Food bank users typically make do with limited financial resources, which is reflected in patterns of food bank use: nearly half (45%) of households who accessed food banks in March 2016 relied on social assistance as their primary source of income. However, Canadians who earn the majority of their income through paid labour are also accessing food banks, accounting for 15% of those assisted in the same month.
Whether it comes as a result of improving the health or increasing the wealth of Canadians, access to the quality and quantity of food we need is essential for living well and reaching our full potential.
This is an edited and updated version of an article that was originally featured in Transition magazine in spring 2013 (Vol. 43, No. 2).
Nathan Battams is responsible for publications, communications and social media at the Vanier Institute of the Family.
Putting the “F” in EFAP: The Evolution of Workplace Mental Health Supports
Craig Thompson
Over the past several decades, mental health has become an increasingly popular topic in public discourse, fuelled in part by our increased understanding of the many ways it affects all levels of society. When people experience changes to their mental health, their family members – always at the “front lines” – are typically the first ones to feel the effects. Family is society’s most adaptable institution. Families respond by adjusting to meet the needs of their members as best they can. In light of this, a growing number of organizations have offered assistance to employees and their families through Employee and Family Assistance Programs (EFAPs) to manage mental health in the workplace. By looking at the evolution of these services, we can learn how and why the “F” in EFAP first emerged, and how it has grown in importance over time.
The early years: Occupational Alcoholism Programs (OAPs)
Occupational Alcoholism Programs (OAPs) were first introduced in Canada in the late 1950s. Predecessors of the EFAPs, they were focused primarily on alcohol and the devastating impact alcohol has on the health and well-being of employees who experience dependency. These programs were typically delivered through the occupational health and medical departments of large industrial organizations in the manufacturing sector.
Employees would sometimes seek out these services through their own initiative, but more often than not were assisted or referred by their manager, supervisor or union steward. The focus of assistance was almost solely on the individual and the alcohol, and did not include the family. The dependent employee would be put on a strict program that included attending Alcoholics Anonymous meetings, and their compliance would be closely monitored. If the individual relapsed after this treatment, it would usually lead to termination and no further support was provided by the employer. Their future would then depend solely on what level of support their family members could muster – if they were still around.
The formative years: Employee Assistance Programs (EAPs)
During the 1970s and mid-1980s, employers expanded the scope of these programs beyond alcohol, and they became known as Employee Assistance Programs (EAPs). Previous research on occupational productivity had shown that alcohol dependency was just one of many issues that could have an impact on a person’s performance, productivity and health in the workplace.
Although alcohol addiction was still seen as a problem, it became increasingly clear that workplace programs could benefit from including support for other issues that can affect productivity, such as other addictions, mental illness, serious health conditions or major life events such as births and deaths. More employers began to understand the value of offering EAPs and, as a result, mid-size, regional, national and global companies introduced programs in their organizations.
EAPs would typically offer short-term, solution-focused counselling, paid for by the employer, with either an average number of sessions or a predetermined maximum number of sessions allotted. EAPs were never intended to provide longer-term care, but when that was necessary, the provider would make a referral to an affordable and appropriate resource. EAPs were increasingly managed by human resources (HR) instead of occupational health and safety or medical departments.
During their prime working years, many people face concerns about their mental health, which EFAPs can help them to manage. Studies have shown that mental health conditions are not only costly to individuals, but also to the organizations to which they belong:
• Depression will rank second only to heart disease as the leading cause of disability worldwide by the year 2020.
• Disability represents anywhere from 4% to 12% of payroll costs in Canada; mental health claims (especially depression) have overtaken cardiovascular disease as the fastest-growing category of disability costs in Canada.
Some employers also started to understand the importance of families in the equation of employee attendance, concentration and focus. Emotional distress, family/personal relationships, child care, eldercare and health care started to get employers’ attention. Many began reaching out directly to family members at home to increase awareness and usage, and to help mitigate the negative impacts of these issues on performance and productivity. Communication materials were specifically designed for spouses and dependants, and creative methods were used to reach out to family members. Program admission was further expanded to include eligible young adults and family members who were attending post-secondary education institutions.
At first, utilization of these programs and services by families remained low, prompting further attempts to increase awareness and usage. One of the factors that limited their use was the fear that personal information would be shared with a counsellor or EAP practitioner and have consequences for the employee at work. Although EAP services were confidential (and remain so), the concerns about confidentiality and privacy protection understandably impaired users from taking advantage of services. During this period, 5% to 7% of the employee population accessed EAP services on any given year, with less than 1% attributed to family members.
While the first generation of EAPs was delivered by internal staff (usually MDs and occupational health nurses), this new generation of programs was typically outsourced to external firms that provided a broader range of professionals and specialty practitioners, including psychologists, counsellors and other health providers. This contributed to broadening the legitimacy of EAPs; however, these programs were still being offered primarily by larger companies and therefore were not yet mainstream. As a result, those who did not work for these firms were typically underserved.
The growth years: Employee and Family Assistance Programs (EFAPs)
The late 1980s through the mid-1990s were marked with important progress in this field. First, EAPs started providing an ever-expanding array of services, including responses for addictions, family/marital relations and psycho-emotional issues. These “broadbrushed” EAPs also recognized the importance of providing services for work relationship issues, financial, legal, aging parent and other non-work-related concerns. With this expansion in scope, EAPs began to take greater hold across a broad range of industries, sectors and workplaces.
Over time, a growing body of research demonstrated that investments by employers in EAPs resulted in various cost benefits, including reduced absenteeism, lower turnover, fewer medical costs and overall higher employee productivity. With this data, EAP providers were able to engage an increasing number of employers of various sizes in other industries to implement an EAP. The level of acceptance grew considerably and, with it, thousands of families and individuals gained access to resources and care.
Providers began offering toll-free 24/7 access to counsellors to eliminate barriers to reaching assistance if and when it was needed. Increased efforts to reach out to the homes of employees did increase family member utilization; however, in most programs, dependant use averaged 5% to 10% of the total utilization. Attention was also now being given to prevention and health promotion through the provision of resource materials, workshops and seminars. Stress management workshops were a central part of the education efforts, with the goal of giving participants the knowledge and tools to remain healthy and productive at work. EAPs also expanded to include services related to dealing with conflict in the workplace, managing workloads realistically and communicating effectively.
Current EFAP Referral Patterns: Percentage of Calls Received, by Issue
45% Marital and family problems
25% Psychological (depression, anxiety, self-image)
15% Work-related problems
10% Substance abuse/alcohol abuse
5% Personal trauma/crisis
Another major step during this phase was the rebranding of Employee Assistance Programs to Employee and Family Assistance Programs (EFAPs). Although most programs had already included the family, this formal change explicitly identified the family as a key stakeholder in the provision of services. Credit needs to be given to the stewards of the MacMillan Bloedel EFAP for having the wisdom and vision to be this apparent and inclusive. They were the first to coin this term, which has become the standard reference for these types of services in Canada. This simple insertion spurred on greater interest in program enhancements for the family into the next phase of evolution.
The maturing years: Today’s EFAPs
From the mid-1990s to today, EFAPs have grown in popularity to the extent that most large and mid-size employers offer some form of program. Even smaller employers (i.e. fewer than 50 employees) have started to offer programs through group plans or community initiatives. This has been largely due to the partnerships that have developed between EFAP providers and group insurance providers in which the group plan can include the EFAP as another option for employers to offer. A range of counselling models (assessment and referral, short-term counselling, etc.) surfaced, varying depending on the organizational culture, industry and program in question. Employers had more models to choose from. During this phase, a wider range of services was made available by telephone, face to face or, more recently, online.
Online services increased accessibility, as they could be reached outside of the workplace from mobile devices and personal computers. This mode of access has increased the use by family members, and future expansion is expected. Online resources such as educational modules on parenting, communicating emotion, enriching relationships and dealing with aging parents are all now common offerings and can be accessed at home or on the road.
Prevention and health promotion has recently expanded to include wellness. A growing number of employers are assisting employees (and their families) to take charge of their overall health, including emotional, psychological and physical well-being. Health risk appraisals (HRAs) have become increasingly available; individuals can benchmark their current health risks and learn how to reduce those risks. Many employers are taking a holistic approach to employee health and wellness, and they are recognizing the importance of the family unit in maintaining and enhancing healthy choices and decisions. Overall employee health is increasingly seen as a vital part of an organization’s “bottom line” thanks to a growing body of research demonstrating direct links between employee well-being and rates of engagement, absenteeism and productivity.
Costs of Mental Illness in the Workplace
- In any given week, more than 500,000 Canadians are absent from work because of mental illness.
- More than 30% of disability claims and 70% of disability costs are attributed to mental illness.
- Approximately $51 billion each year are lost to the Canadian economy because of mental illness.
Current and emerging legal requirements are now compelling greater numbers of employers to ensure that their workplaces are psychologically safe and built on relationships of civility and respect. In 2013, the federal guidelines for the National Standard of Canada for Psychological Health and Safety in the Workplace were introduced to help organizations actively work toward creating psychologically healthy and safe environments for employees.
This standard was developed using evidence-based research from a variety of scientific and legal disciplines; it outlines existing knowledge on the psychological health and safety of workers, and provides guidelines and recommendations for promoting and maintaining healthy workspaces. While the standard is voluntary, there is still an obligation for employers to provide some degree of care based on current and evolving legislation and case law. As Dr. Martin Shain, who has written extensively on psychological safety in the workplace, says, “A psychologically safe workplace is no longer a nice to do, but is now a must do.”
The future of EFAPs
In the early days, when services focused on alcoholism, employers could readily fire an employee for non-compliance. In today’s climate, whether in response to legislation or regulations, or in compliance with voluntary standards, more employers are providing access to professional assistance and treatment to address the myriad of mental and physical conditions that may disable or impair an employee. After an employee reaches out seeking treatment, employers are taking greater steps to accommodate his or her return to work. As the dialogue on the reduction of stigma surrounding these issues grows in volume and intensity, more workers, families and communities are getting assistance.
The evolution of EFAPs demonstrates a growing interest within organizations to integrate care for the employees, ensuring that family circumstances are considered and enabled. Whether the result of legal obligation or efforts to increase performance and productivity, or out of care for employee well-being, a growing number of employers now take psychological health and safety in the workplace seriously. As interest and investment in EFAPs and employee well-being grows, further breakthroughs are bound to occur. Although it is difficult to anticipate with great accuracy what the future of employee assistance may look like, families will most likely remain a central component of future approaches.
This article can be downloaded in PDF format by clicking here.
Craig Thompson, MEd, MBA, has been a clinician, business developer, account manager and business leader in the field of EFAP and Disability Management for nearly three decades. Over this period, he has worked with thousands of employers and employees and their families with a purpose of improving their lives and enhancing workplace effectiveness.
Modern Maternity Care in Canada
Cecilia Benoit
Georgina, a mother of Mi’kmaq heritage, is in the last stage of her pregnancy. Reluctantly, she is preparing to leave her home community of Port-aux-Basques, located on the southwestern tip of Newfoundland, to give birth in the only remaining maternity hospital in her health region, the Western Memorial Regional Hospital in Corner Brook, 220 kilometres away from her family and friends. Her chances of having a maternity doctor or midwife she knows attend her birth are slim to none, and there is a 30% chance that her baby will be delivered by Caesarean section.
Millennium Development Goal 5, to improve maternal health, is one of the United Nations Millennium Development Goals (MDGs). Of the eight MDGs, the least progress has been made toward the right of every woman to the best possible maternity care. Indigenous, poor and rural and remote women such as Georgina are especially compromised. While Canada made major strides throughout the 20th century to improve maternal health and build a universal maternity care system, many shortcomings remain, including but not limited to the medicalization of childbirth and inequitable access to maternity providers.
History of childbirth in Canada
Pregnancy and childbirth are significant life events in all cultures. In earlier times, midwives were the primary care providers. Care during pregnancy typically took place in the local community and birth occurred in the home.
Medicalization of maternity care in Canada, while significantly predating the development of the modern welfare state, became enshrined and solidified within the package of policies and regulations that accompanied the adoption of universal health care, known as “medicare,” which was implemented and formally adopted in 1972.
While Canada’s health care model is often referred to as a simple single payer health care system, funding and delivery of insured services are in fact much more complex. They involve federal and provincial/territorial governments, community services, private insurance companies and individuals.
Most physicians work in private practice, with their services paid from the provincial/territorial insurance plans. Funding for the insurance plans comes from the general revenues of the provinces/territories, with additional transfer payments from the federal government through the Canada Health and Social Transfer or, more recently, the Canada Health Transfer.
Under medicare, only physician-provided maternity care services were covered by the public health care system, which resulted in shifting the role of midwives (women) to medical doctors (mostly men). In the publicly funded health care system that was created, physicians also retained their right to remain private entrepreneurs, establishing their practices wherever they deemed appropriate.
The system created through medicare did not address the pre-existing disparity in the availability of physician services and solidified the hospital as the control centre of the maternity care system. Due to concerns about modesty and fear of contagion, it also excluded partners and other kin from participating in the age-old event of childbirth.
Modern childbirth in Canada
By the early 1980s, virtually all women across the country were delivering their babies in regional hospitals, attended by a maternity physician or obstetrician and assisted by obstetrical nurses. But these institutional changes left women lonely and new fathers sidelined. Research shows that women who have the support of a partner during labour require less pain relief and feel more positive about the birth. As research began to show the importance of healthy parent–child attachment, the health care system responded by allowing partners to be active participants in the birthing process. Partners today are present for the majority of births, taking on a greater role not only in these first moments of their children’s lives, but also with child rearing and household management in the years that follow.
Maternal deaths rose in Canada from 6 to 12 per 100,000 births between 1990 and 2013.
In 2013, UNICEF ranked Canada 22nd out of 29 high-income countries for infant mortality rates, with the rate substantially higher among Indigenous peoples.
Canada currently boasts the lowest maternal mortality rate in the American continent, reflecting improvements throughout the 20th century in women’s education, their nutrition, control of their fertility and universal coverage of physician services. Yet maternal deaths rose in Canada from 6 to 12 per 100,000 births between 1990 and 2013. By contrast, Japan and a number of European countries today have mortality rates half the Canadian rate or lower. Equally disconcerting, in 2013, UNICEF ranked Canada 22nd out of 29 high-income countries for infant mortality rates, with the rate substantially higher among Indigenous peoples.
In recent decades, the number of family doctors involved in maternity care delivery has significantly declined, as has the number of hospitals offering maternity care services. At the same time, the percentage of deliveries attended by obstetricians has increased substantially; for example, obstetricians currently attend 80% of hospital births in Ontario.
Caesarean section rates have also steadily increased, with the total national rate increasing from 17.6% in 1995 to 22.5% in 2001, and 27.3% in 2013 (see table below). The current rate of Caesarean section births ranges from a high of 32% in British Columbia and 31% in Newfoundland and Labrador to a low of 23.1% in Saskatchewan and 21.41% in Manitoba. According to the World Health Organization, Caesarean section rates below 10% indicate underuse of this life-saving procedure, while rates above 15% are deemed to show overuse. Overuse of Caesarean section has been linked to higher morbidity in mothers, including an increased risk for depression and post-traumatic stress, lower breastfeeding rates and a greater likelihood of future complications in pregnancy. Despite popular media images of maternal demand for Caesarean section, there is little evidence that the increase in the national rate in the last 20 years, and the even more surprising current cross-country variation, is based on mothers’ demand for a convenient pain-free birth – the so-called “too posh to push” argument.
Modern midwifery in Canada
Beginning with Ontario, British Columbia and Quebec in the 1990s, and spreading across most other regions since, midwives have received formal education and become regulated, and their services have been publicly funded. Yet the occupation still remains unregulated and unfunded in Newfoundland and Labrador, Yukon, Prince Edward Island and New Brunswick. Moreover, only 9% of births in Canada are currently attended by a midwife. While the percentage of midwife-attended births is higher in some regions (e.g., 19% in British Columbia), the demand outstrips the supply, with a substantial proportion of women in all parts of the country wanting access to a trained, publicly funded midwife but unable to find one.
Women with lower education, younger mothers, women without a partner and women living in rural and remote areas or socio-economically disadvantaged communities have the least access to publicly funded midwifery services. The Association of Ontario Midwives estimates that as many as 40% of women who want to see a midwife in Ontario are currently unable to find one, and women in other provinces are also experiencing frustration trying to find midwifery care. Following developments in Quebec and Manitoba, Ontario recently funded two free-standing, midwifery-led birth centres. Yet this option is not available for many non-Indigenous and Indigenous women, such as Georgina mentioned above, who instead experience loneliness, disconnection from their local maternity traditions and isolation from family; the overall result is “stressful births.”[ii]
Modern postpartum care in Canada
The length of time Canadian women spend in hospital following childbirth has decreased dramatically during the modern period, from a mean of five days in 1984–85 to just less than two days after vaginal delivery today. Hospital stays are costly; early hospital discharge for mothers and their newborns helps administrators control or reduce obstetrical care expenditures. For some women with strong support systems and access to publicly funded physician or midwifery services, early discharge from hospital is usually a welcomed occasion.
As in earlier times, family support can be crucial in the postpartum period. Fathers and/or partners across Canada, with the support of parental leave policies, are playing a much bigger role after childbirth than in previous generations – a shift in family roles that continues to this day. According to Statistics Canada, 31% of recent fathers across the country claimed or intended to take parental leave in 2013 – a significant increase from 3% in 2000. The rate is much higher in Quebec, particularly since the introduction of the Quebec Parental Insurance Plan (QPIP), which is the only plan in the country that specifically provides paternity leave. Since the introduction of QPIP in 2006, uptake has almost tripled, from 28% in 2005 to 83% in 2013.
But for women without these familial and formal options, the result can lead to negative health outcomes for themselves and their infants. Provincial and territorial health care systems cover a limited range of postnatal care services. At the federal level, this has traditionally been restricted to the provision of informational supports by the provinces and the publication of national guidelines for maternity and newborn care. In some regions, an optional home visit by either a public health nurse or a lay home visitor is still available, while in other regions, services following discharge from hospital have been reduced to a telephone call to a new mother from a public health nurse.
Privately delivered postnatal services have emerged to fill this care gap. There currently exist no published research studies on the for-profit postnatal services that currently exist in Canada. Postpartum doulas who advertise online often propose tangible, high-intensity supports such as newborn care, breast- and bottle-feeding support, child-minding services, meal preparation, household chores and so on. Unfortunately, relatively high out-of-pocket costs make these forms of support accessible only to those who are able to pay for them. Doulas who advertise online generally charge around $25 per hour, or anywhere from $100 to $1,000 for overnight or week-long package deals, respectively. Research studies in this emerging area of practice are needed to determine the scope of practice and outcomes for mothers and their families. There is currently no information available on user demographics, patterns of use or outcomes associated with these forms of commodified care, though such information would offer insight into the types and levels of unmet needs that exist.[iii]
The future of maternity care in Canada
As is clear from our history, midwives were the main maternity care providers in what is now Canada before the arrival of European settlers and up to the modern period. Midwives provided not only crucial technical care, but also social support to enhance the health and well-being of women and babies in homes and local communities. Modernization of maternity care involved the move from midwives and natural childbirth into the medicalization of childbirth, with obstetricians replacing family doctors as the maternity providers, and labour and delivery restricted to fewer and fewer hospitals. High Caesarean rates and the associated unnecessary morbidity for mothers is one outcome of this modern system of care. The return to midwifery and the integration of midwives into our health care system have thus far been insufficient, as midwives are too few in number, they are concentrated in urban centres and their services are not equally available in all provinces/territories.
As the country works toward achieving MDG 5, as families become more complex and partners become more involved in childbirth and child care, and as we have access to more research on how to increase positive health outcomes for mothers and newborns, the health care system will continue to evolve and adapt to ensure the availability and effectiveness of maternity care in our communities from coast to coast to coast.
Cecilia Benoit, PhD, is a Scientist at the Centre for Addictions Research of British Columbia, Professor in the Department of Sociology at the University of Victoria and former co-leader of the Women’s Health Research Network. She is also recipient of the 2016 Governor General’s Awards in Commemoration of the Persons Case.
Download this article in PDF format.
SOURCES
[i] Cecilia Benoit et al., “Medical Dominance and Neoliberalisation in Maternal Care Provision: The Evidence from Canada and Australia,” Social Science & Medicine, 71:3 (August 2010), accessed August 24, 2015. http://bit.ly/1Jv2r5j.
[ii] Cecilia Benoit et al., “Maternity Care as a Global Health Policy Issue,” The Palgrave International Handbook of Healthcare Policy and Governance, Ellen Kuhlmann, Robert H. Blank, Ivy Lynn Bourgeault and Claus Wendt (Eds.). Basingstoke: Palgrave, 2015. http://bit.ly/1NPii1r.
[iii] Cecilia Benoit et al., “Privatisation & Marketisation of Post-birth Care: The Hidden Cost for New Mothers,” International Journal for Equity in Health, 11:1 (October 2012). http://bit.ly/1ikd1BS.
Dads Play a Greater Role at Home: Family Life Benefits
Nathan Battams
(Updated March 21, 2016)
As Canadians prepare to celebrate Father’s Day, modern fathers, grandfathers and great-grandfathers are redefining what exactly fatherhood means to families and society. Canada’s 8.6 million increasingly diverse dads are taking on a greater role in their children’s lives. This evolution in fatherhood has had positive impacts inside and outside the family home.
“This is one of the biggest social changes in our time,” says Vanier Institute of the Family CEO Nora Spinks. “The ‘Leave it to Beaver’ family model accounts for fewer and fewer of Canada’s families as family forms and relationships become more diverse and complex.”
There’s no question that fatherhood has become more diverse over the past 50 years. A growing share of Canada’s dads was born outside the country, bringing with them ideas of what fatherhood means. More same-sex couples are raising children, one in five being male couples. Over the past two decades, there has been an increase in lone-parent families headed by men. The number of indigenous fathers is growing at a faster rate than those in the general population. This evolution of Canada’s family portrait means that there is no single “fatherhood experience.”
The classic father figure has traditionally been portrayed as an emotionally distant figure whose primary role was to earn the family income. This depiction overlooks the diversity that has always existed. Historically, many women have played a role in managing family finances and generating income inside and outside the paid labour force. In 1976, one-third of Canadian families with at least one child under age 16 had two earners in the paid labour force. By 2014, this accounted for 55% of these families.
A growing number of dads now play a bigger role in their children’s lives. In fact, an increasing number of dads are leaving the breadwinning to their partners altogether so they can focus on raising children. In 2014, 11% of single-earner families with a “stay-at-home” parent had a father who was staying at home – up from only 1% in 1976.
Whether they’re working or not, fathers are spending more time with their families than in the past. According to Statistics Canada, men spent 360 minutes per workday with family members in 1986. By 2010, this reached 379 minutes. Three-quarters of surveyed Canadian dads say that they’re more involved with their children than their father had been with them.
Fathers who decide to play a greater role in the lives of their children aren’t anomalies. In a recent study comparing parental leave in Quebec with the rest of Canada, author Ankita Patnaik found that when given the option, most men embrace paternal leave. Since 2006, the Quebec Parental Insurance Plan (QPIP) has offered non-transferable leave for men, making Quebec the only province where father-specific leave is available.
Patnaik found that before QPIP, Quebec fathers took an average two weeks of leave. After the parental leave policy was reformed, the average Quebec father took the full five weeks available under the paternity leave program. In addition, the share of Quebec fathers taking parental leave jumped from 27.8% in 2005 to 78.3% in 2014. Outside Quebec, only 9.4% of recent dads report taking leave.
Patnaik’s study also found that in Quebec, there was a “large and persistent impact” on gender dynamics in the three-year period following parental leave. Fathers remained more likely to do housework, while mothers were more likely to engage in paid work. Quebec dads also spent an average half-hour more per day at the family home.
Father involvement can have a positive impact on child development and well-being. Literature reviews from the Father Involvement Research Alliance (FIRA) have found many benefits of “highly involved” fathers. Children in these families experience higher levels of cognitive development and resilience. They tend to perform better in school. They also report higher levels of life satisfaction and psychological well-being.
Modern fathers continue their involvement in the lives of their children even after a marriage or common-law relationship has come to an end. More than one-third of divorced or separated parents share or alternate major decision making related to their children. Nearly one-quarter (24%) of divorced or separated parents report that their children either spend equal time living with mom and dad, or live primarily at the father’s residence.
In a 2014 report from the Involved Father and Gender Equity Project, interviews with new fathers revealed that family life benefited from their expanding involvement. Many said that their entry into fatherhood was a “transformational journey” that gave them a new outlook on life and relationships. They also reported that greater participation in housework and child-rearing promoted equality within their relationships. Many said that community supports and connections with other fathers encouraged their increased involvement.
“While modern fatherhood today consists of many diverse experiences, today’s generation of fathers is certainly taking on a greater, broader role in family life than in the past,” says Spinks. “As they’re sharing the breadwinning role, spending more time with family and taking more parental leave, these dads are changing what fatherhood means in Canada.”
Nathan Battams is a writer and researcher at the Vanier Institute of the Family
Suggested Reading: “‘I Don’t Have Time for This!’: A Compassionate Guide to Caring for Your Parents and Yourself”
By Katherine Arnup, PhD
Aging, illness and dying are realities that we all will face at some point, in our family circles and ultimately in our own lives. Despite this fact of life, most people in the Western world are hesitant to discuss this inevitable journey with our loved ones, despite the importance of these conversations in preparing for the future.
In her new book, “I Don’t Have Time for This!”: A Compassionate Guide to Caring for Your Parents and Yourself, award-winning author Dr. Katherine Arnup provides a thoughtful and informative guide to beginning essential conversations with our parents about the end of life, tools and strategies for caregiving, keys to releasing guilt and regret, advice about asking for and receiving help, and the positive impact that facing aging, illness and death can have on our lives (and those around us).
“Katherine Arnup has been able to capture the complexity of life and living in family relationships while guiding us gently through the inevitability of death and dying. Documenting both sides of the caregiving/receiving experience, this important and timely resource helps us summon the courage to have the sometimes difficult conversations with loved ones and service providers – and with ourselves. A validation for those who have been a part of an end-of-life experience and an inspiration for all of us who expect to be part of one in the future – even if it is only our own.” – Nora Spinks, CEO, Vanier Institute of the Family
To learn more about the family experiences of death and dying in the Canadian context, read Death, Dying and Canadian Families – a 2013 report by Dr. Arnup, published as part of the Vanier Institute’s Contemporary Family Trends series. This report explores the death denying/defying culture of the Western world and its implications for families in Canada while rooting the discussion in four key contexts: Canada’s aging population, the realities of chronic illness and the need for care, the gap between desires and reality regarding the location of death, and the impact on families and family life.
About Katherine Arnup, PhD
Katherine Arnup is a social historian, life coach and retired university professor. She is the author of the award-winning book Education for Motherhood: Advice for Mothers in Twentieth-Century Canada, editor of the first book on lesbian families in Canada (Lesbian Parenting: Living with Pride and Prejudice) and author of more than three dozen articles on marriage, motherhood, lesbian and gay families, aging, death and dying.
Strength in Diversity: Positive Impacts of Children with Disabilities
Michelle R. Lodewyks
When it comes to exploring the experiences of families raising children with disabilities, studies tend to focus on the perceived negative impact of the disability on the family. These families are commonly viewed as “victims” who face excessive caregiving demands, emotional distress, physical and/or financial burdens and interpersonal difficulties, while the children are portrayed primarily as sources of stress and anguish. This tragedy dialogue supports an assumption that families with children with disabilities experience “chronic sorrow” and perpetuates the perception of disability as something to be avoided or eradicated. These perceptions have a major influence on today’s assumptions about – and reactions to – disability, including how professionals respond to children with disabilities and how society views and responds to children at birth. Consequently, the general public tends to overlook many positive impacts and meaningful contributions that children with disabilities make within their families, communities and society in general.
In order to explore the positive impact disability can have within families, a qualitative, interview-based study was performed to add narrative depth to the research. All of the parents and children interviewed identified a variety of positive effects the children have had on their families and contributions the children have made to family life. The most unsurprising discovery was the affirmation that a child with a disability can have some of the same positive effects on their families and make some of the same contributions as any other child. Highlighting these similarities is critical, given the tendency for children with disabilities to be distinguished from other children and viewed as less likely to affect their families in positive ways. Yet perhaps even more meaningful was the discovery that children with disabilities can also have unique positive effects and make unique contributions to families and family life.
Raising a child with a disability provides opportunities for personal growth
Parents in the study reported an ability to more readily recognize and appreciate the value, potential and strengths of a person with a disability as a result of their parenting experiences. Many described how their experiences left them with a greater acceptance of diversity, a stronger belief that there is an inherent and intrinsic value in people and a “more balanced appreciation for what people are about.”
One participant said her experience gave her a new perspective on how to help individuals she works with; she learned not to place limits on people or tell them what they can or cannot do, but instead help them strive for self-improvement. Siblings of children with a disability experienced attitudinal changes brought about by this family relationship. For these siblings, increased exposure to disability in their family environment made them more comfortable around other children with a disability, and they discovered a new-found enthusiasm for getting to know people with disabilities in general.
Children with a disability often exceeded expectations and did not necessarily comply with what is typical for their diagnoses, often being nothing close to the worst-case scenarios predicted by some doctors. As one participant stated, “I don’t know what my parents would have thought about people with disabilities before I came around, but I think it’s just… shown them that it really doesn’t mean that much… you can still be productive and still have goals and not really let anything stop you, as hard as that is sometimes.”
All of the parents in the study perceived themselves as having acquired new or enhanced positive character attributes as a result of raising a child with a disability. Attribute changes included family members learning to open their hearts and to be more loving, warm, caring, creative, balanced, gentle, calm, outgoing, responsible, independent and less selfish.
The positive attribute change most commonly reported by parents of a child with a disability was that they became more tolerant and accepting. As family members learned to be more accepting of diversity and of people’s behaviours, they cultivated a greater respect for other families of children with disabilities and experienced more compassion toward people in general.
Several parents commented that their child made them an overall “better person,” “better parent” or made other family members “better people.” Some of these effects carried over into the workplace: one participant perceived himself as a “better person at work” because of the understanding his son has given him about autism. This understanding has enabled him to relate to staff and other people in a different way; he supports his colleagues by helping them understand and interpret the behaviour of a co-worker who also has autism.
Parents experience pride, joy and strengthened relationships
All parents in the study reported positive emotions their children have fostered in them. A sense of pride was the most common. One parent recognized that some of the things that evoke a sense of pride “may not be the same as what other people [her son’s age] are doing,” yet she maintained she had numerous reasons to be proud. Parents expressed pride in, or were impressed by, their children’s knowledge or creativity, their sense of right and wrong, their methods for overcoming fears, their ability to put their minds to something and take a chance, and for being their own advocates. Additionally, all 10 children reported the positive emotions they also felt they evoked in family members – more than half believing they made their family proud.
One mother insisted she derives more excitement from the little things in life than many other people and that she “celebrate[s] things that other people don’t even think about celebrating” because of her daughter. Another explained her pride in her daughter as follows: “Disability-wise, I’m very proud of her because she hasn’t let her disability control her life. She’s got multiple disabilities… And she doesn’t let that slow her down… It would be too easy to say, ‘Oh, I can’t do this’ and give up… She’s always willing to push the limits and do the best that she can.”
Many parents talked about having met people, gained friendships and made new connections thanks to their child. While any child can expand a family’s social network, certain examples were attributed to the family’s particular circumstances. For one couple, connecting themselves to other families through the creation of a support network for parents with similar experiences has been valuable, as they have been able to offer support to other parents who have approached them for advice and guidance.
Despite one parent noting that having a child with a disability may make some families “fall apart,” many parents perceived that their child strengthened their marriage or made the parents and/or family stronger. Two of the parents felt they had become better at communicating and sharing with their spouse thanks to their child. The father in this couple talked about the difficulty he and his wife experienced when their son was first diagnosed and described the role each played in helping the other get through the “tough parts.” Their experience, he explained, has made him and his wife “more free to talk about things and feelings,” thus improving their communication.
A few parents mentioned how their child added a fresh perspective and/or insight to the family. One father commented on the value of his son’s insight and identified this as something he appreciates most about him: “His insight into things is so different than anybody else. He thinks differently than we do… and I love hearing his insight. He adds such a dimension to our house… I just can’t imagine not having that dimension in our home. It’s… such a core of who we are in this house. He’s so amazing.”
Referring to his natural gifts when it comes to writing and composing music, one of the children insisted that having autism has given him the ability to be hyperfocused and successful with music. He concluded, “I think the music is a positive impact. It can impact everyone else, too, if they hear it.”
When asked how she makes a difference in her family, another one of the children replied, “I suppose it would be a little less lively without me. There wouldn’t be as many interesting dinner conversations.” She also referred to “the whole yin and yang thing” and how she counterbalances the mellowness in her family.
Families learn from their unique experiences and seek to share their knowledge
Before concluding the interviews, all participants were asked what they would like other people to understand about them, their family and/or their experience. Parents shared that their experiences are “not all rosy” – that there have been “challenges,” “struggles,” “obstacles” and “tough times.” Yet parents did not necessarily hold the child responsible for any negative aspects of their experience. One parent admitted that her struggles adjusting to her child’s disability had less to do with the child than with other people’s preconceptions and the parents’ own feelings regarding what their experience would be like. She explained, “There was no question, that period of time where you struggle with it – a bit of a denial thing. Well, you almost grieve, but you come to the conclusion that those feelings are more about you, and what you thought, or what other people might be thinking.”
Other parents agreed that any anger, stress, anxiety and/or crises they may have experienced resulted from having to deal with the ignorance of other people and a general lack of societal understanding rather than from the child. One mother requested that people reconsider their use – or misuse – of certain labels, explaining that, while people with intellectual disabilities are often labelled as hindered in some way, “the hindrance is very often on the so-called ‘normal’ people for lack of understanding them.”
These findings coincided with those from an earlier study in which parents suggested that the sorrow they experienced originated largely from having to deal with recurring messages of negativity and hopelessness from other people, such as professionals, the health system, other family members and friends. This suggests a source of stress and negativity outside the child and that a family’s perceptions about their child may be determined, at least in part, by the surrounding cultural beliefs about disability. Therefore, if society holds negative attitudes toward disability and the surrounding cultural perceptions are largely negative, negativity can be transmitted to the family – to parents’ views of, and beliefs about, their children and to their parenting.
The parents in the study also wished to dispel negative assumptions others might associate with their child and place any negativity in context of the bigger picture. Some described their experience “as a gift instead of a burden,” and insisted it is not a source of anything negative to have a child with a disability in the family, emphasizing that they are not sorry for the way their child has changed their lives. While acknowledging the stress, hard work and commitment required to raise a child with a disability, other parents commented on the unfortunate nature of other people not realizing how rewarding the experience can be. One father reframed his experience raising his son in the following way: “You want a catastrophe? You want tragedy? You know what, let me pick up a paper and show you about somebody who died in a car accident. Let me show you about a young mother that was killed. Let me show you about the tsunami. Those are tragedies. This is a curveball. All you’ve got to do is learn how to hit curves and you’ll be fine… And it’s not easy, but you learn to grow with it.”
Among the most common requests from parents were that assumptions not be made based on disability and that people recognize each child’s ability and potential. Parents insisted that their children can give a lot to society and deserve respect and requested that people make an effort to learn from their children. Elaborating, one parent cautioned, “I was just thinking in terms of the impact of… people with Down syndrome on the world… We’ve been trying to basically eradicate this group of people by all the blood testing and stuff. It devalues the lives that they have. And they have something to offer… They’ve got something really special that we need to sit up and take note of because we could learn a lot from them.”
When asked what they wanted to share with others, similarly powerful messages came from the children. One of the children wanted others to “understand that I have disabilities, but I’m not a worse person for it.” Another child offered the following take-away message: “Lots of people have the perception that I’m kind of slow… I want them to know that I really do know a lot about the world and what’s going on, and it hasn’t stopped me – having cerebral palsy, being in a wheelchair – I’m not an unaware person. I have big ambitions and a bright future. I don’t want them to feel sorry for me, because I think I’m going to have a really good and interesting and fun life!”
The positivity of embracing diversity goes beyond the family
Learning from families who view their circumstances in a positive light, making these perceptions more readily available to the general public and coming to view the experience of raising a child with a disability as one that is not necessarily tragic – but rather enriching and rewarding – can have a variety of positive implications. These findings can provide medical professionals (particularly those involved in prenatal screening and diagnosis) with practical information to share with families when a diagnosis is given. These findings might also benefit other parents currently raising a child with a disability by encouraging them to focus more closely on what their child adds to their life.
In presenting these findings, this study is not denying the existence of challenges and negative family experiences. Sharing these findings is also not suggesting that everything will automatically improve for families who struggle raising a child with a disability. Yet the belief is that appreciating the strengths and positives has potential for beneficial change. There is also evidence that focusing on the children’s positive impacts and contributions may serve to control the meaning and level of stress associated with the experience. This could be helpful in the adaptation process. If more families see their experiences in a positive light, perhaps they can assist in altering widespread perceptions of the impact of disability, provide support to new parents and relieve some of the fear and anxiety around the idea of raising a child with a disability. In doing so, the hope is that a more affirmative way of viewing disability could be promoted.
Michelle Lodewyks is an Instructor in the Disability and Community Support Program at Red River College as well as a graduate of the Master’s Program in Disability Studies at the University of Manitoba.
SOURCES
Fotheringham, J. B., Skelton, M., & Hoddinott, B. (1971). The Retarded Child and His Family: The Effects of Home and Institution. Toronto, ON: Institute for Studies in Education.
Gupta, A., & Singhal, N. (2004). Positive Perceptions in Parents of Children with Disabilities. Asia Pacific Disability Rehabilitation Journal, 15:1. http://bit.ly/ZSm1oU (accessed October 9, 2014).
Kearney, P. M., & Griffin, T. (2001). Between Joy and Sorrow: Being a Parent of a Child with Developmental Disability. Journal of Advanced Nursing, 34:5.
Kharasch Behr, S. (1989). Underlying Dimensions of the Construct of Positive Contributions That Individuals with Developmental Disabilities Make to Their Families: A Factor Analytic Study. University of Kansas (unpublished doctoral dissertation).
Pearlin, L. I., & Schooler, C. (1978). The Structure of Coping. Journal of Health and Social Behavior, Vol. 19.
Stainton, T., & Besser, H. (1998). The Positive Impact of Children with an Intellectual Disability on the Family. Journal of Intellectual and Developmental Disability, 23:1. http://bit.ly/1s01wQt (accessed October 9, 2014).
Summers, J. A. (1988). Family Adjustment: Issues in Research on Families with Developmentally Disabled Children. In V. B. Van Hasselt, P. S. Strain and M. Hersen (Eds.), Handbook of Developmental and Physical Disabilities. Elmsford, NY: Pergamon.
Swain, J., & French, S. (2000). Towards an Affirmation Model of Disability. Disability & Society, 15:4. http://bit.ly/1ycgl7r (accessed October 9, 2014).
Whitney, D., & Trosten-Bloom, A. (2003). The Power of Appreciative Inquiry: A Practical Guide to Positive Change. San Francisco, CA: Berrett-Koehler Publishers, Inc.
Woolfson, L. (2003). Disabled Children, Parents and Society – A Need for Cognitive Reframing. Proceedings of the British Psychological Society, 11:1. http://bit.ly/1uGHSuW (accessed October 9, 2014).