
Research Snapshot: The Value and Distribution of Family Caregiving in Canada
A summary of a study about the economic value and distribution of caregiving

A summary of a study about the economic value and distribution of caregiving
RAPP and the Vanier Institute have published a compilation of caregiving infographics.

Research on Aging, Policies and Practice has published new data on the economic contributions of

Research on Aging, Policies and Practice provides new data on the “business case” for supporting
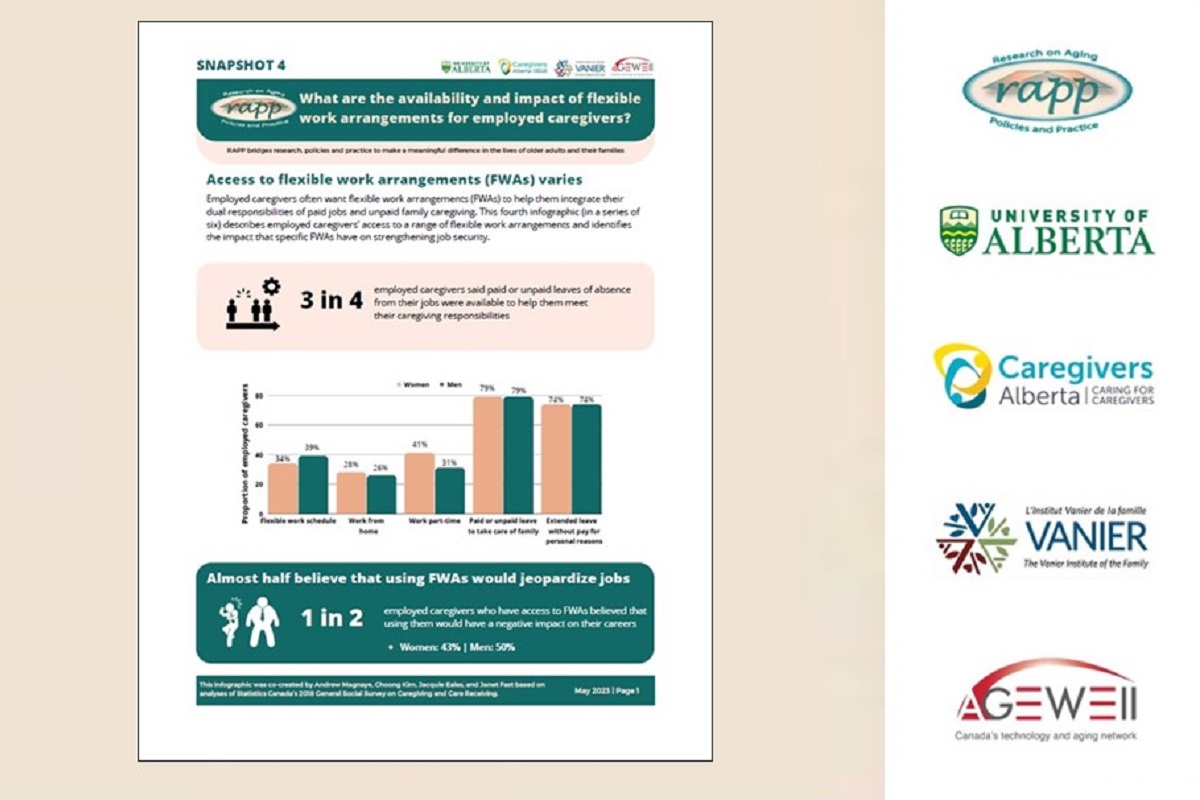
Research on Aging, Policies and Practice has published new data on the availability and impact

Research on Aging, Policies and Practice has published new data on how caregiving affects employed
Highlights from a study exploring the experiences of employed Indigenous caregivers

Findings from a survey on the experiences and talents of employed caregivers

Findings from a study on caregiving experiences of newcomer families in Canada

Research on Aging, Policies and Practice has published new data on how caregiving affects employed

Research on Aging, Policies and Practice has published new data on working caregivers.

Fast facts on family care for National Caregiver Day 2022.

This event is now closed.

Gaby Novoa summarizes new research on the impact of workplace policies on employed caregivers.
A summary of a study about the economic value and distribution of caregiving
RAPP and the Vanier Institute have published a compilation of caregiving infographics.
Research on Aging, Policies and Practice has published new data on the economic contributions of
Research on Aging, Policies and Practice provides new data on the “business case” for supporting
Research on Aging, Policies and Practice has published new data on the availability and impact
Research on Aging, Policies and Practice has published new data on how caregiving affects employed
Highlights from a study exploring the experiences of employed Indigenous caregivers
Findings from a survey on the experiences and talents of employed caregivers
Findings from a study on caregiving experiences of newcomer families in Canada
Research on Aging, Policies and Practice has published new data on how caregiving affects employed
Research on Aging, Policies and Practice has published new data on working caregivers.
Fast facts on family care for National Caregiver Day 2022.
This event is now closed.
Gaby Novoa summarizes new research on the impact of workplace policies on employed caregivers.
613-228-8500 | info@vanierinstitute.ca
94 Centrepointe Dr., Ottawa ON K2G 6B1 Canada
© 2024 The Vanier Institute of the Family

The Vanier Institute of the Family is located on the unceded territory of the Algonquin Anishinaabe people, who have protected this land since time immemorial and who continue to live and work here today. We strive to support decolonization by amplifying voices and research that highlight the ongoing impacts of colonialism, displacement, and systemic racism on Indigenous family and community connections, cultures, and wellbeing.
Learn more
613-228-8500
94 Centrepointe Dr., Ottawa ON K2G 6B1 Canada
© 2023 The Vanier Institute of the Family